Automated Registry Monitoring Speeds Clinical Safety Surveillance
By HospiMedica International staff writers
Posted on 15 Feb 2017
A new study claims that implementing automated, web-based surveillance of medical devices can help spot potential safety problems with less delay.Posted on 15 Feb 2017
Researchers at Lahey Hospital and Medical Center, Vanderbilt University Medical Center, and other institutions conducted a prospective, propensity-matched study to evaluate a strategy of active surveillance of the U.S. CathPCI Registry to evaluate the Cardinal Health Mynx extravascular vascular-closure device (VCD), implanted following percutaneous coronary intervention (PCI) procedures with femoral access.
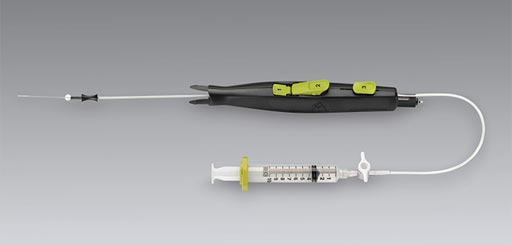
Image: The Mynx VCD has a higher risk of vascular complications than other VCDs (Photo courtesy of Cardinal Health).
The researchers used an integrated clinical-data surveillance system to compare the Mynx device with alternative VCDs, with the primary outcome being any vascular complication, a composite of access-site bleeding, access-site hematoma, retroperitoneal bleeding, or any vascular complication requiring intervention. Secondary end points were access-site bleeding requiring treatment and postprocedural blood transfusion. In all, the researchers analyzed data from 73,124 patients who received Mynx devices from January 1, 2011, to September 30, 2013.
The results showed the Mynx device was associated with a significantly greater risk of any vascular complication (1.2%) than were alternative VCDs (0.8%); there was also a significantly greater risk of access-site bleeding and transfusion. The relative risks were greater in three pre-specified high-risk subgroups: patients with diabetes, those 70 years of age or older, and women. The initial alerts occurred within the first 12 months of monitoring, and were confirmed in an independent sample of 48,992 patients. The study was published on January 25, 2017, in the New England Journal of Medicine (NEJM).
“The takeaway is we were able to detect a safety signal fairly quickly. When it comes to post-market safety surveillance for medical devices, you have to be really timely in your safety alerting for it to matter,” said senior author professor of biomedical informatics, medicine, and biostatistics Michael Matheny, MD, MPH, MS. “In our world, nine months is quick enough that if you could get the signal to the FDA, they could act on it.”
The surveillance system developed is called DELTA, for Data Extraction and Longitudinal Trend Analysis, and is freely available as open-source software. The system performs automated safety analyses and comparative effectiveness studies prospectively, as patient outcomes are electronically documented and uploaded to the system. When DELTA finds potential safety issues, it sends alerts to users via email. DELTA can be adapted for surveillance of medical devices and drugs, and for quality profiling of clinical services and individual clinicians.














