Immune Response to Trauma May Predict Organ Failure
By HospiMedica International staff writers
Posted on 25 Jul 2017
Early gene response during the initial two hour window following trauma could help determine which patients will later develop multiple organ dysfunction syndrome (MODS), according to a new study.Posted on 25 Jul 2017
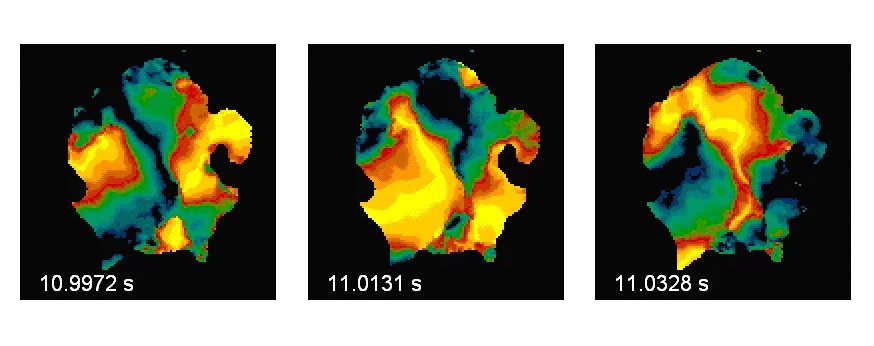
Researchers at Queen Mary, University of London (QMUL; United Kingdom) and University College London (UCL, United Kingdom) performed whole blood transcriptome and flow cytometry analyses in 70 critically injured patients during the hyperacute time period (within two hours of injury), comparing transcriptome findings in 36 critically injured patients with those of six patients with minor injuries. They then performed flow cytometry analyses in the other 34 critically injured patients and compared findings with those of nine healthy volunteers.
They found that immediately after injury, only 1,239 gene transcripts (4%) were differentially expressed in the critically injured patients; but 24 hours later, a “genomic storm” involving 6,294 transcripts (21%) were differentially expressed. However, only 202 (16%) of those genes differentially expressed in the hyperacute window were still expressed in the same direction at 24 hours post-injury. Pathway analysis showed principally up-regulation of pattern recognition and innate inflammatory pathways, with down-regulation of adaptive responses.
When the researchers compared the immune cell genes expressed in patients who later developed MODS to those who did not, most differences were seen immediately after injury, where 363 genes had different activity levels between MODS and non-MODS patients, compared to only 33 genes remaining after 24 hours. According to the researchers, the results suggest a central role for neutrophils and Natural Killer (NK) cells, with under-expression of T- and B cell responses, in determining development of MODS. The study was published on July 12, 2017, in PLOS Medicine.
“The first minutes or hours after a traumatic injury is a key window where a patient's immune response may set the trajectory for whether they develop organ failure,” said lead author Professor Karim Brohi, MD, of the QMUL Centre for Trauma Sciences. “This phase is very challenging to study due to the complexity and logistics of the emergency environment, but if we can understand the mechanisms that lead to poor outcomes, we may be able to help bring dramatic improvements through better diagnostics and therapeutics.”
An excessive, inappropriate, or dysfunctional immune response leads to cellular injury and MODS, including damage to the lungs, kidney, liver, and cardiovascular failure. Patients with MODS require intensive care support as it has a high mortality and morbidity rate, and also affects long-term health outcomes. Pathogenesis remains unclear, and several models have been proposed, such as excessive inflammation, a second-hit insult, or an imbalance between pro- and anti-inflammatory pathways.
Related Links:
Queen Mary, University of London
University College London












.jpg)