3D-Printed Porous Tantalum an Emerging Material for New Generation of Orthopedic Implants
Posted on 07 Nov 2024
Bones are the hard organs that form the endoskeleton of vertebrates, featuring a complex inner and outer structure that allows them to maintain hardness while minimizing weight. Their roles include facilitating movement, providing structural support, protecting the body, producing red and white blood cells, and storing essential minerals. However, incidents, diseases, and aging can lead to fractures, bone defects, and joint degeneration, necessitating the use of artificial metallic orthopedic implants. Consequently, there is a growing interest in developing effective metallic orthopedic implants through innovative material design. Now, researchers have published a review in the International Journal of Extreme Manufacturing that offers a thorough overview of 3D-printed porous tantalum (pTa), a promising material for replacing bone defects in orthopedic implants.
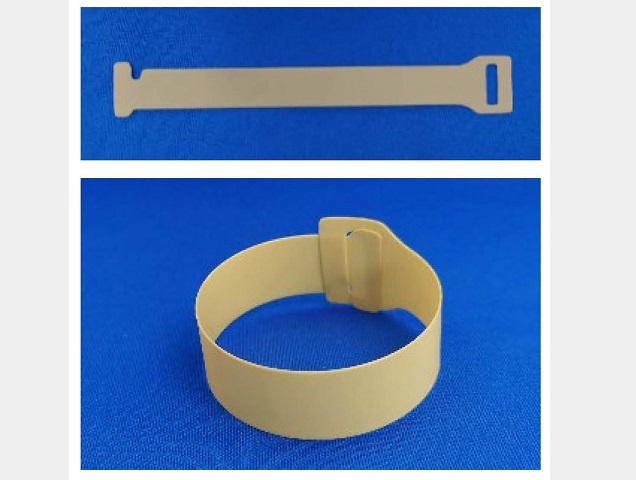
This review, conducted by researchers at Central South University (Changsha, China), focuses on enhancing the bioactivity of pTa implants through material design, providing insights into how such design can innovate orthopedic implants. It presents a detailed discussion of recent advancements in pTa materials for implant development, including various designs based on surface morphology, pore structure, alloying, and functional modifications. The review also addresses potential limitations concerning in vitro cellular bioactivity, in vivo animal osseointegration, and the clinical application of pTa implants. Notably, pTa exhibits an elastic modulus comparable to that of bone, which helps to minimize the shielding effect while offering adequate physiological support for new bone tissue with high strength.
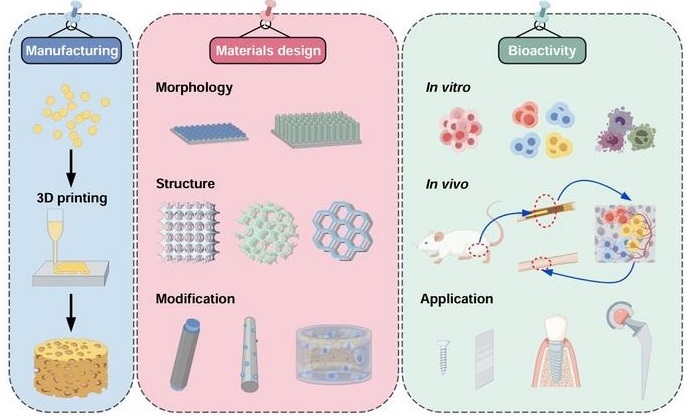
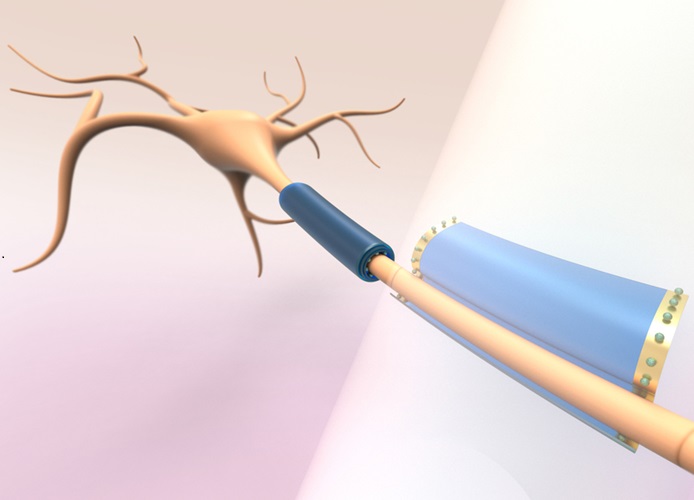
Moreover, its friction-resistant properties contribute to enhanced initial stability. The porous structure of pTa, which mimics that of natural bone, promotes cell adhesion, vascularization, and nutrient exchange, facilitating inward bone growth and osseointegration. To manufacture functional products with improved bioactivity, pTa orthopedic implants must adhere to fundamental standards, including mechanical properties, biocompatibility, and biosafety, all of which can be achieved through specialized material design. Additionally, addressing the osseointegration of pTa orthopedic implants in complex human environments with diseases is crucial, as these implants should support the surrounding tissues while allowing bone to integrate into the material. The design considerations depend on the complexity of the bone defect site, its anatomical location, and the desired clinical outcomes.
Despite considerable progress in pTa orthopedic implants, producing complex pTa bone implants that strike an optimal balance between morphological structure (such as micro-nano surfaces, pore shape, size, and porosity), mechanical properties (including elastic modulus, fatigue performance, and wear resistance), and biological characteristics (such as bioactivity and biocompatibility) remains a challenge. In postoperative rehabilitation, the correct positioning and design of implants can significantly enhance patient recovery outcomes and quality of life. Achieving optimal clinical results will require close collaboration between rehabilitation physicians and surgeons to assess each patient’s unique circumstances, ensuring that the implants satisfy mechanical and biological requirements while also accommodating individual anatomical features and rehabilitation needs.
Furthermore, while researchers often focus on improving the biocompatibility and osseointegration of Ta-based implants, they sometimes overlook the stability and durability of these materials under biomechanical stress and force variations in the implanted body. This oversight can affect biological evaluations in animal studies and delay clinical applications. Therefore, expediting the assessment of the stability and durability of Ta-based implants under dynamic mechanical conditions in animal experiments is another critical aspect for advancing clinical application. Although challenges remain, researchers have charted a path forward for the development of orthopedic implants.
“The preparation and application of future orthopedic implants will not just be a matter of biomedical engineering, but a highly interdisciplinary approach involving advanced technologies from various disciplines (e.g., Artificial Intelligence (AI), Virtual Reality (VR), Augmented Reality (AR), and 5G technologies) interacting with the clinical team,” stated Prof. Mingchun Zhao.












.jpg)