New Material Aids Facial Skin Reconstruction
|
By HospiMedica International staff writers Posted on 11 Aug 2011 |
An injectable composite of biological and synthetic molecules shows promise in restoring damaged soft tissue relatively safely and durably.
Researchers at Johns Hopkins University (Baltimore, MD, USA) created the new composite material from hyaluronic acid (HA), a natural component in skin of young people that confers elasticity, and polyethylene glycol (PEG), a synthetic molecule used successfully as surgical glue in operations and known not to cause severe immune reactions. The PEG can be cross-linked-- forming sturdy chemical bonds between many individual molecules--using energy from light, which traps the HA molecules with it. Such cross-linking makes the implant hold its shape and not dissipate away from the injection site.
To develop the best PEG-HA composite with the highest long-term stability, the researchers injected different concentrations of PEG and HA under the skin and into the back muscle of rats, used a green light emitting diode (LED) light to gel the material, and then used magnetic resonance imaging (MRI) to monitor the persistence of the implant over time. The MRIs and direct measurements of the implants showed that the ones created from HA and the highest tested concentration of PEG with HA remained the same size over time, compared to injections of only HA, which shrank over time.
The researchers also evaluated the safety and persistence of the PEG-HA implants in three volunteers undergoing abdominoplasty. Technicians injected about five drops of PEG-HA or HA alone under the belly skin. The participants said they sensed heat and pain during the gel setting process; 12 weeks after implantation, MRI revealed no loss of implant size in patients. Removal of the implants and inspection of the surrounding tissue revealed mild to moderate inflammation, a response similar to that seen in the rats, although the types of white blood cells (WBCs) responding to implant differed between the rodents and humans. The difference was attributed to the fact that the target tissue in the rats (muscle) was different than human belly fat. The study was published in the July 27, 2011, issue of Science Translational Medicine.
“Implanted biological materials can mimic the texture of soft tissue, but are usually broken down by the body too fast, while synthetic materials tend to be more permanent but can be rejected by the immune system and typically don’t meld well with surrounding natural tissue,” said lead author Prof. Jennifer Elisseeff, MD, PhD, director of the Translational Tissue Engineering Center at JHU School of Medicine. “Our composite material has the best of both worlds, with the biological component enhancing compatibility with the body and the synthetic component contributing to durability.”
“Many of the skin fillers available on the market consisting of HA-like materials used for face lifts are only temporarily effective, and are limited in their ability to resculpt entire areas of the face,” added Professor Elisseeff. “Our hope is to develop a more effective product for people, like our war veterans, who need extensive facial reconstruction.”
Related Links:
Johns Hopkins University
Researchers at Johns Hopkins University (Baltimore, MD, USA) created the new composite material from hyaluronic acid (HA), a natural component in skin of young people that confers elasticity, and polyethylene glycol (PEG), a synthetic molecule used successfully as surgical glue in operations and known not to cause severe immune reactions. The PEG can be cross-linked-- forming sturdy chemical bonds between many individual molecules--using energy from light, which traps the HA molecules with it. Such cross-linking makes the implant hold its shape and not dissipate away from the injection site.
To develop the best PEG-HA composite with the highest long-term stability, the researchers injected different concentrations of PEG and HA under the skin and into the back muscle of rats, used a green light emitting diode (LED) light to gel the material, and then used magnetic resonance imaging (MRI) to monitor the persistence of the implant over time. The MRIs and direct measurements of the implants showed that the ones created from HA and the highest tested concentration of PEG with HA remained the same size over time, compared to injections of only HA, which shrank over time.
The researchers also evaluated the safety and persistence of the PEG-HA implants in three volunteers undergoing abdominoplasty. Technicians injected about five drops of PEG-HA or HA alone under the belly skin. The participants said they sensed heat and pain during the gel setting process; 12 weeks after implantation, MRI revealed no loss of implant size in patients. Removal of the implants and inspection of the surrounding tissue revealed mild to moderate inflammation, a response similar to that seen in the rats, although the types of white blood cells (WBCs) responding to implant differed between the rodents and humans. The difference was attributed to the fact that the target tissue in the rats (muscle) was different than human belly fat. The study was published in the July 27, 2011, issue of Science Translational Medicine.
“Implanted biological materials can mimic the texture of soft tissue, but are usually broken down by the body too fast, while synthetic materials tend to be more permanent but can be rejected by the immune system and typically don’t meld well with surrounding natural tissue,” said lead author Prof. Jennifer Elisseeff, MD, PhD, director of the Translational Tissue Engineering Center at JHU School of Medicine. “Our composite material has the best of both worlds, with the biological component enhancing compatibility with the body and the synthetic component contributing to durability.”
“Many of the skin fillers available on the market consisting of HA-like materials used for face lifts are only temporarily effective, and are limited in their ability to resculpt entire areas of the face,” added Professor Elisseeff. “Our hope is to develop a more effective product for people, like our war veterans, who need extensive facial reconstruction.”
Related Links:
Johns Hopkins University
Latest Surgical Techniques News
- Novel Endoscopy Technique Provides Access to Deep Lung Tumors
- New Study Findings Could Halve Number of Stent Procedures
- Breakthrough Surgical Device Redefines Hip Arthroscopy
- Automated System Enables Real-Time "Molecular Pathology" During Cancer Surgery
- Groundbreaking Procedure Combines New Treatments for Liver Tumors
- Ablation Reduces Stroke Risk Associated with Atrial Fibrillation
- Optical Tracking Method Identifies Target Areas in Robot-Assisted Neurosurgery
- General Anesthesia Improves Post-Surgery Outcomes for Acute Stroke Patients
- Drug-Coated Balloons Can Replace Stents Even in Larger Coronary Arteries
- Magnetic Kidney Stone Retrieval Device Outperforms Ureteroscopic Laser Lithotripsy
- Absorbable Skull Device Could Replace Traditional Metal Implants Used After Brain Surgery
- Magic Silicone Liquid Powered Robots Perform MIS in Narrow Cavities
- 'Lab-on-a-Scalpel' Provides Real-Time Surgical Insights for POC Diagnostics in OR
- Biodegradable Brain Implant Prevents Glioblastoma Recurrence
- Tiny 3D Printer Reconstructs Tissues During Vocal Cord Surgery
- Minimally Invasive Procedure for Aortic Valve Disease Has Similar Outcomes as Surgery
Channels
Critical Care
view channel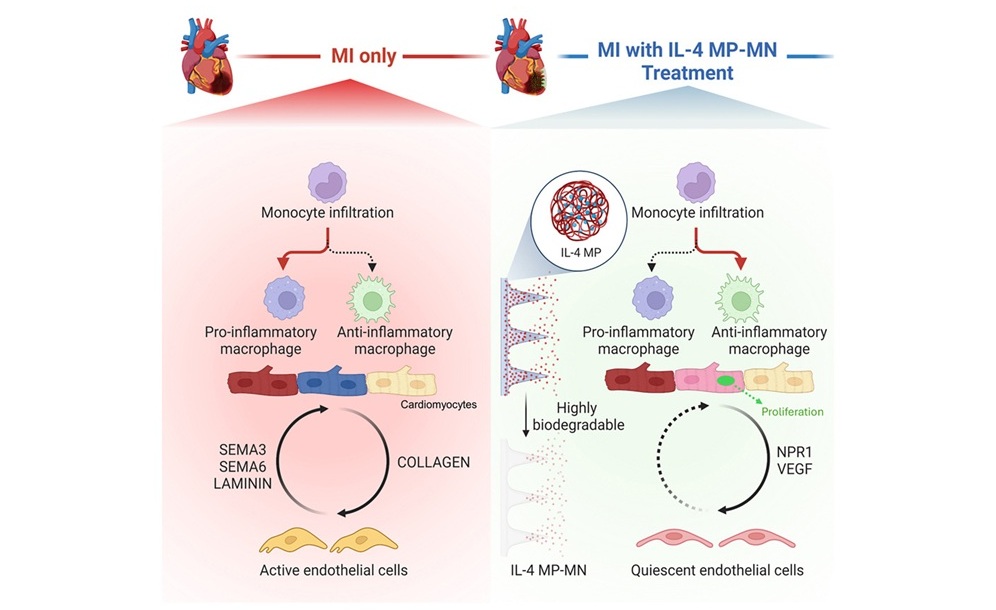
Biodegradable Patch Repairs Damaged Tissue After Heart Attack
A heart attack causes sudden loss of oxygen to the heart muscle, triggering cell death and a strong inflammatory response that often leads to scar formation. While scarring helps stabilize the heart, it... Read more
Magnetically Guided Microrobots to Enable Targeted Drug Delivery
Stroke affects 12 million people globally each year, often causing death or lasting disability. Current treatment relies on systemic administration of clot-dissolving drugs, which circulate throughout... Read more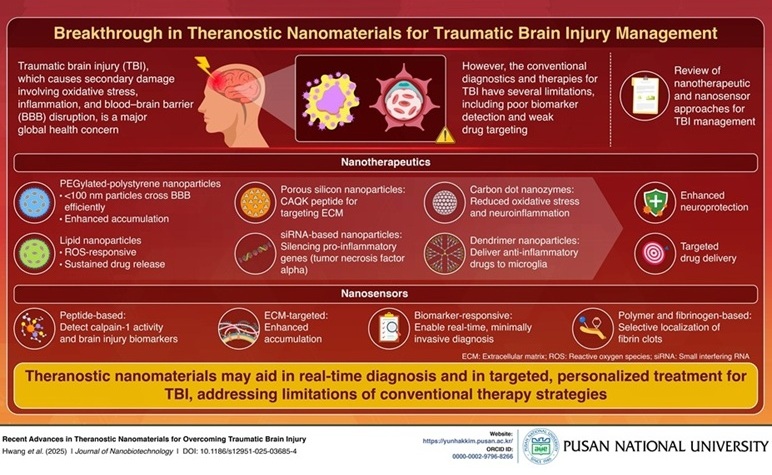
Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
Traumatic brain injury (TBI) continues to leave millions with long-term disabilities every year. After a sudden impact from a fall, collision, or accident, the brain undergoes inflammation, oxidative stress,... Read more
Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
Blood loss during or after surgery can place significant stress on people with heart disease, increasing the risk of dangerous complications. Transfusions are often delayed until hemoglobin levels fall... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more












