Esophageal Stent Alleviates Benign Strictures
|
By HospiMedica International staff writers Posted on 06 Mar 2014 |

Image: The WallFlex Nitinol esophageal stent (Photo courtesy of Boston Scientific).
A fully covered metal stent provides new treatment options for patients with benign narrowing of the esophagus.
The WallFlex esophageal stent is made of a nickel-titanium (Nitinol) wire braided construction that provides luminal patency in the presence of strictures or benign tumors. The stent is designed for gradual expansion, typically complete in 24-72 hours; it features a Permalume silicone coating that is designed to prevent tumor in-growth, seal concurrent esophageal fistulas, and help reduce food impaction. The WallFlex Stent also provides physicians with clear visualization during fluoroscopy, aiding in accurate placement, as well as progressive, step flared ends that assist in anchoring the stent within the esophageal lumen.
An additional feature is a Teflon coated polyester suture that enables easy removal for up to eight weeks, potentially saving patients from having to visit the hospital to undergo additional dilations. The WallFlex Esophageal Fully Covered Stent is a product of Boston Scientific (Natick, MA, USA), and has received the European Community CE marking of approval. The stent is not approved for the removal from malignant strictures and has not been approved in the United States for the treatment of refractory benign esophageal strictures.
“Building on the best of Boston Scientific's industry-leading stents, the expanded indication for the WallFlex Esophageal Fully Covered Stent demonstrates our commitment to physician needs and dedication to improving patient outcomes,” said David Pierce, president of endoscopy at Boston Scientific. “This enables physicians in the European Union to provide additional options for the treatment and management of patients suffering from benign esophageal strictures.”
“Fully covered esophageal stents are a valid therapeutic option in patients with benign refractory esophageal strictures,” said Javier Jimenez, MD, chief of the Endoscopy Department at Complejo Hospitalario de Navarra (Pamplona, Spain). “I use the WallFlex Esophageal Stent because its small profile and radiopacity facilitate accurate placement, the migration rate is low, and stent removal is usually easy.”
Benign esophageal strictures are a narrowing or tightening of the esophagus caused by scarring that cause swallowing difficulties. Strictures can be caused by or associated with gastroesophageal reflux disease (GERD), esophagitis, a dysfunctional lower esophageal sphincter, disordered motility, lye ingestion, or a hiatal hernia. Strictures can also form after esophageal surgery and other treatments such as laser therapy or photodynamic therapy (PDT). The primary treatment is dilation of the esophagus, which may need to be repeated after a period if the stricture recurs.
Related Links:
Boston Scientific
The WallFlex esophageal stent is made of a nickel-titanium (Nitinol) wire braided construction that provides luminal patency in the presence of strictures or benign tumors. The stent is designed for gradual expansion, typically complete in 24-72 hours; it features a Permalume silicone coating that is designed to prevent tumor in-growth, seal concurrent esophageal fistulas, and help reduce food impaction. The WallFlex Stent also provides physicians with clear visualization during fluoroscopy, aiding in accurate placement, as well as progressive, step flared ends that assist in anchoring the stent within the esophageal lumen.
An additional feature is a Teflon coated polyester suture that enables easy removal for up to eight weeks, potentially saving patients from having to visit the hospital to undergo additional dilations. The WallFlex Esophageal Fully Covered Stent is a product of Boston Scientific (Natick, MA, USA), and has received the European Community CE marking of approval. The stent is not approved for the removal from malignant strictures and has not been approved in the United States for the treatment of refractory benign esophageal strictures.
“Building on the best of Boston Scientific's industry-leading stents, the expanded indication for the WallFlex Esophageal Fully Covered Stent demonstrates our commitment to physician needs and dedication to improving patient outcomes,” said David Pierce, president of endoscopy at Boston Scientific. “This enables physicians in the European Union to provide additional options for the treatment and management of patients suffering from benign esophageal strictures.”
“Fully covered esophageal stents are a valid therapeutic option in patients with benign refractory esophageal strictures,” said Javier Jimenez, MD, chief of the Endoscopy Department at Complejo Hospitalario de Navarra (Pamplona, Spain). “I use the WallFlex Esophageal Stent because its small profile and radiopacity facilitate accurate placement, the migration rate is low, and stent removal is usually easy.”
Benign esophageal strictures are a narrowing or tightening of the esophagus caused by scarring that cause swallowing difficulties. Strictures can be caused by or associated with gastroesophageal reflux disease (GERD), esophagitis, a dysfunctional lower esophageal sphincter, disordered motility, lye ingestion, or a hiatal hernia. Strictures can also form after esophageal surgery and other treatments such as laser therapy or photodynamic therapy (PDT). The primary treatment is dilation of the esophagus, which may need to be repeated after a period if the stricture recurs.
Related Links:
Boston Scientific
Latest Surgical Techniques News
- Minimally Invasive Coronary Artery Bypass Method Offers Safer Alternative to Open-Heart Surgery
- Injectable Breast ‘Implant’ Offers Alternative to Traditional Surgeries
- AI Detects Stomach Cancer Risk from Upper Endoscopic Images
- NIR Light Enables Powering and Communicating with Implantable Medical Devices
- Simple Bypass Protocol Improves Outcomes in Chronic Cerebral Occlusion
- Implantable Absorbable Sensor Detects Life-Threatening Complications After Intestinal Surgery
- New Study Findings Enable Improved Ventilation During Complex Lung Surgery
- 3D-Printed Blood Vessel Scaffolds Could Transform Heart Bypass Surgeries
- Novel Imaging Technique Helps View Blood Perfusion During Esophageal Surgery
- Minimally Invasive Surgery Proven Safe and Effective for Complex ‘Whipple’ Procedure
- Catheter-Based Procedures Offer Less Invasive Option for Treatment of Valvular Disease
- Laparoscopic Surgery Improves Outcomes for Severe Newborn Liver Disease
- Novel Endoscopy Technique Provides Access to Deep Lung Tumors
- New Study Findings Could Halve Number of Stent Procedures
- Breakthrough Surgical Device Redefines Hip Arthroscopy
- Automated System Enables Real-Time "Molecular Pathology" During Cancer Surgery
Channels
Critical Care
view channel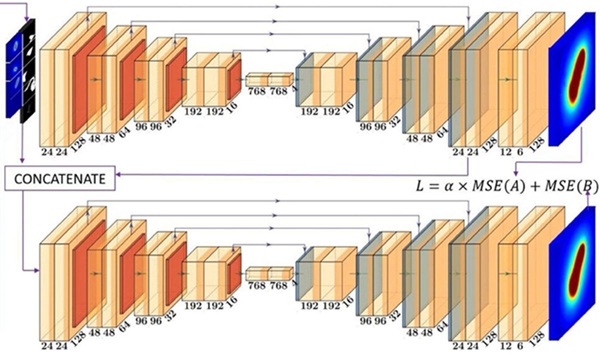
AI Tool Improves Speed and Accuracy of Cervical Cancer Treatment Planning
Cervical cancer affects around 600,000 women globally each year and causes approximately 340,000 deaths. Brachytherapy is among the most effective treatments for this cancer, but its use is often limited... Read more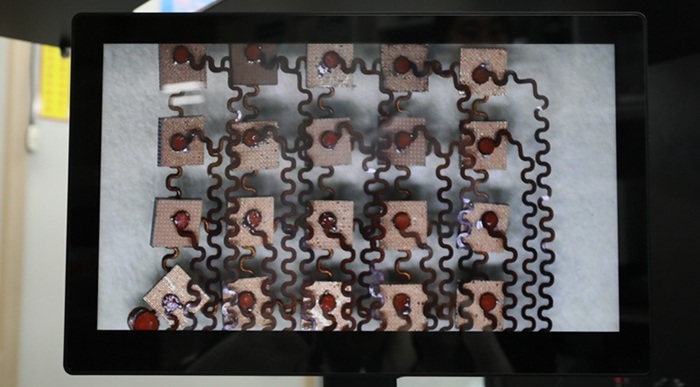
Ultrasonic Sensor Enables Cuffless and Non-Invasive Blood Pressure Measurement
Accurate blood pressure monitoring is essential for managing cardiovascular disease, yet conventional cuff-based systems are bulky, intermittent, and uncomfortable for long-term use. Optical cuffless methods... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more