Heart Association Issues Statement on Understanding Radiation Risks Before Cardiac Imaging
|
By HospiMedica International staff writers Posted on 16 Oct 2014 |

Image: The American Heart Association issued a statement that patients need to be informed on radiation risks before undergoing cardiac imaging (Photo courtesy of AHA - The American Heart Association).
People should understand why a heart-imaging test is needed before undergoing the procedure, including the benefits and risks involved, such as the potential long-term risk from radiation exposure, advises a new scientific statement.
The statement was published online, before print, on September 29, 2014, in the American Heart Association’s (AHA; Dallas, TX, USA) journal Circulation. “When medical imaging is being considered, patients should feel very comfortable asking how the test will help them and the possible risks, including radiation-related risks,” said Reza Fazel, MD, MSc, chair of the writing committee for the statement and an AHA volunteer currently serving on the Joint Cardiac Imaging Committee of the AHA’s Council on Clinical Cardiology and Council on Cardiovascular Radiology.
As technology has evolved, imaging modalities have become an increasingly important application in diagnosing and treating patients with heart disease. However, the rising use has resulted in higher radiation exposure during the last 20 years. Heart imaging now accounts for nearly 40% of the radiation exposure patients receive from medical tests, according to the statement.
“In general, the radiation-related risk of any imaging test to an individual patient is very small and, when the test is clinically appropriate, the benefits of the test typically far outweigh any potential risks,” said Dr. Fazel, a cardiologist at Beth Israel Deaconess Medical Center (Boston, MA, USA).
Some questions that may help a patient understand the risks and benefits are: (1) how will this test help diagnose or treat my heart problem? (2) Will the results of this test change the recommended treatment? (3) Are there other techniques to get the information without using radiation? (4) How much radiation exposure may occur? (5) How could that affect my chance of developing cancer later in life? (6) Lastly, how does that risk compare to the risk from other common activities?
The most typically used heart and blood vessel imaging procedures using radiation are nuclear stress tests, cardiac computed tomography (CT) scans and fluoroscopy (a real-time X-ray technology used to guide catheter and device placement during heart catheterization and tests for heart rhythm abnormalities). Echocardiography and cardiac magnetic resonance imaging do not expose patients to ionizing radiation.
The new statement also provides guidance for the training of professionals who order or administer cardiac imaging tests. Clinicians planning imaging tests should understand when each type of test is appropriate, the typical average radiation dose and the potential risks. In deciding the best imaging method to use, the clinician should also consider the test’s diagnostic accuracy, potential risks, cost, availability, and the patient’s convenience.
“Radiation-related risk is one of the factors that should be considered in the decision to use cardiovascular imaging with ionizing radiation, particularly in younger patients in whom the potential risk of radiation exposure is thought to be higher,” Dr. Fazel said.
Clinicians who perform cardiac imaging should understand current methods required to select the optimal dose of radiation—using enough to produce high-quality imaged, not significantly more than that. They should also know how to minimize radiation exposure to staff, according to the statement.
Related Links:
American Heart Association
Beth Israel Deaconess Medical Center
The statement was published online, before print, on September 29, 2014, in the American Heart Association’s (AHA; Dallas, TX, USA) journal Circulation. “When medical imaging is being considered, patients should feel very comfortable asking how the test will help them and the possible risks, including radiation-related risks,” said Reza Fazel, MD, MSc, chair of the writing committee for the statement and an AHA volunteer currently serving on the Joint Cardiac Imaging Committee of the AHA’s Council on Clinical Cardiology and Council on Cardiovascular Radiology.
As technology has evolved, imaging modalities have become an increasingly important application in diagnosing and treating patients with heart disease. However, the rising use has resulted in higher radiation exposure during the last 20 years. Heart imaging now accounts for nearly 40% of the radiation exposure patients receive from medical tests, according to the statement.
“In general, the radiation-related risk of any imaging test to an individual patient is very small and, when the test is clinically appropriate, the benefits of the test typically far outweigh any potential risks,” said Dr. Fazel, a cardiologist at Beth Israel Deaconess Medical Center (Boston, MA, USA).
Some questions that may help a patient understand the risks and benefits are: (1) how will this test help diagnose or treat my heart problem? (2) Will the results of this test change the recommended treatment? (3) Are there other techniques to get the information without using radiation? (4) How much radiation exposure may occur? (5) How could that affect my chance of developing cancer later in life? (6) Lastly, how does that risk compare to the risk from other common activities?
The most typically used heart and blood vessel imaging procedures using radiation are nuclear stress tests, cardiac computed tomography (CT) scans and fluoroscopy (a real-time X-ray technology used to guide catheter and device placement during heart catheterization and tests for heart rhythm abnormalities). Echocardiography and cardiac magnetic resonance imaging do not expose patients to ionizing radiation.
The new statement also provides guidance for the training of professionals who order or administer cardiac imaging tests. Clinicians planning imaging tests should understand when each type of test is appropriate, the typical average radiation dose and the potential risks. In deciding the best imaging method to use, the clinician should also consider the test’s diagnostic accuracy, potential risks, cost, availability, and the patient’s convenience.
“Radiation-related risk is one of the factors that should be considered in the decision to use cardiovascular imaging with ionizing radiation, particularly in younger patients in whom the potential risk of radiation exposure is thought to be higher,” Dr. Fazel said.
Clinicians who perform cardiac imaging should understand current methods required to select the optimal dose of radiation—using enough to produce high-quality imaged, not significantly more than that. They should also know how to minimize radiation exposure to staff, according to the statement.
Related Links:
American Heart Association
Beth Israel Deaconess Medical Center
Latest Critical Care News
- Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
- Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
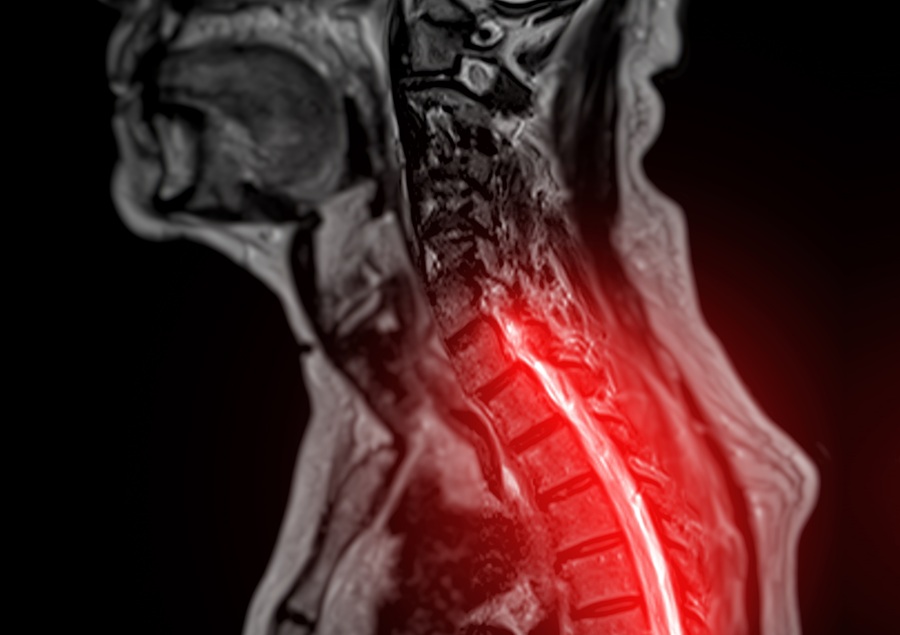
- AI Model Could Help Diagnose Spinal Cord Disease Up To 30 Months Earlier
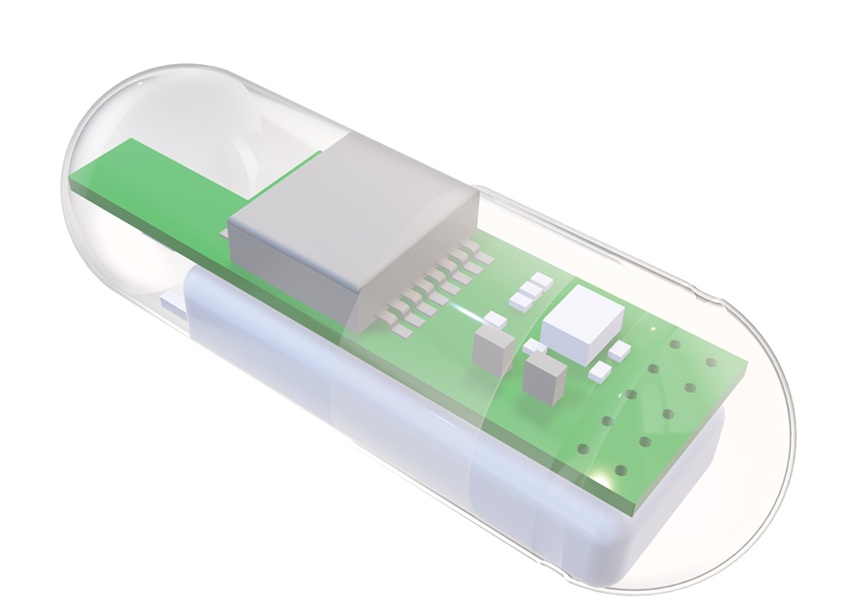
- 3D-Printed Swallowable Robot Could Perform Gastrointestinal Procedures
- Next-Gen Hydrogel Could Transform Soft Tissue and Organ Repair
- Engineered Cancer Eating Bacteria Consume Tumors from Inside Out
- ‘Cyborg’ Transplants Could Replace Pancreatic Tissue Damaged by Diabetes
- Smartphone-Linked Catheter Sensor Spots UTIs Sooner Than Lab Cultures
- AI Tool Identifies Trauma Patients Requiring Blood Transfusions Before Reaching Hospital
- New Clinical Guidelines to Reduce Central Line-Associated Bloodstream Infection
- New Inhalable Treatment for TB Lowers Side Effects
- AI Algorithm Improves Antibiotic Decision-Making in Urinary Tract Infection
- 3D-Printed System Enhances Vaccine Delivery Via Microneedle Array Patch
- Whole-Heart Mapping Technology Provides Comprehensive Real-Time View of Arrhythmias
- Wearable Device for Diabetics Could Replace Continuous Glucose Monitoring Systems
- AI Stethoscope Spots Heart Valve Disease Earlier Than GPs
Channels
Artificial Intelligence
view channelCritical Care
view channel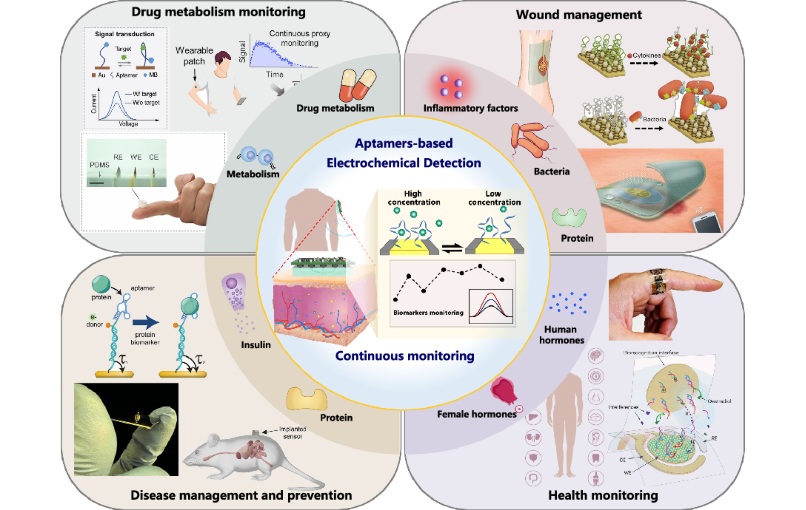
Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
Continuous monitoring of biomarkers is critical for early disease detection, treatment evaluation, and personalized health management. Yet most clinical tests still rely on invasive, single-point blood... Read more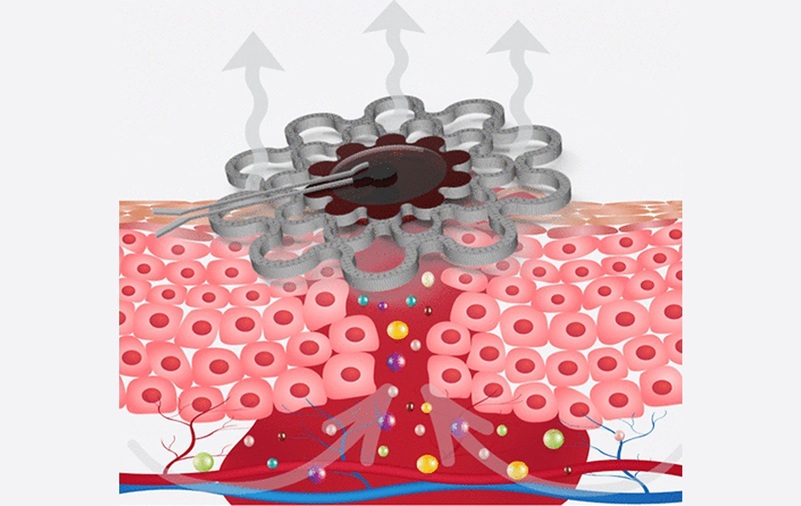
Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
Any wound has the potential to become chronic, but the risk is significantly higher in individuals with certain medical conditions. Once a wound becomes chronic, healing slows, complications increase,... Read moreSurgical Techniques
view channel
Brain Implant Records Neural Signals and Delivers Precise Medication
Neurological diseases such as epilepsy involve complex interactions across multiple layers of the brain, yet current implants can typically stimulate or record activity from only a single point.... Read moreAI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
Lipid-rich plaques inside coronary arteries are strongly associated with heart attacks and other major cardiac events. While optical coherence tomography (OCT) provides detailed images of vessel structure... Read moreNeural Device Regrows Surrounding Skull After Brain Implantation
Placing electronic implants on the brain typically requires removing a portion of the skull, creating challenges for long-term access and safe closure. Current methods often involve temporarily replacing the skull or securing metal plates, which can lead to complications such as skin erosion and additional surgeries.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more