Lung Simulations Could Improve Respiratory Treatment
|
By HospiMedica International staff writers Posted on 02 Aug 2015 |
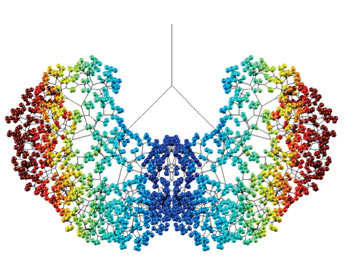
Image: Computer model of SRT delivered to an adult human lung; blue areas receive less (Photo courtesy of Prof. James Grotberg/U-M Engineering).
An innovative computer model that predicts the flow of liquids in human lungs could provide insight into the treatment of acute respiratory distress syndrome (ARDS).
ARDS is a life-threatening inflammation of the respiratory system that kills 74,000 adults each year in the United States alone. It is most common among patients with lung injury or sepsis, a whole-body inflammation caused by infection. Treatment involves surfactant replacement therapy (SRT) to make it easier for the lungs to inflate, similar to the therapy used in premature babies, who can lack the surfactant necessary to expand their lungs. While SRT has contributed to a dramatic reduction in mortality rates of premature babies, the attempt to implement the technology in adults has been largely unsuccessful.
To try and reveal why, researchers at the University of Michigan (U-M; Ann Arbor, USA) and Ecole Polytechnique (Palaiseau, France) developed a mathematical computer model that provided a three-dimensional (3D) image of exactly how SRT flowed through the lungs of patients in the three key trials that examined the technology. The first (1997) clinical study in adults showed promise, cutting mortality rate from 40% to 20%. But two larger studies in 2004 and 2011 showed no improvement in mortality, and the treatment was abandoned.
The computer model used fluid mechanical principals for 3-D modeling of the lung airway tree in both neonates and adults, showing how a liquid plug propagates through the tree from forced inspiration. In two separate modeling steps, they saw that the SRT plug deposits a coating film on the airway wall, and then splits unevenly at the bifurcation due to gravity. The model generates 3D images of the resulting acinar distribution and calculates two global indexes, efficiency and homogeneity.
When the researchers applied this engineering perspective to SRT, they saw one detail that set the successful 1997 study apart; a less concentrated version of medication was used. The SRT used in the 1997 study delivered the same dose of medication as the later studies, but it was dissolved in up to four times more liquid. The additional liquid helped the medication reach the tiny air sacs in the lungs. The study was published on July 13, 2015, in Proceedings of the National Academy of Sciences of the United States of America (PNAS).
“The medication needs to work its way from the trachea to tiny air sacs deep inside the lungs to be effective. This therapy is relatively straightforward in babies but more complex in adults, mostly because adult lungs are much bigger,” said lead author professor of biomedical engineering James Grotberg, MD, PhD, of the U-M College of Engineering. “The modeling technology could be used in other types of research as well, including more precise targeting of other medications in the lungs and projecting results from animal research to humans.”
Related Links:
University of Michigan
Ecole Polytechnique
ARDS is a life-threatening inflammation of the respiratory system that kills 74,000 adults each year in the United States alone. It is most common among patients with lung injury or sepsis, a whole-body inflammation caused by infection. Treatment involves surfactant replacement therapy (SRT) to make it easier for the lungs to inflate, similar to the therapy used in premature babies, who can lack the surfactant necessary to expand their lungs. While SRT has contributed to a dramatic reduction in mortality rates of premature babies, the attempt to implement the technology in adults has been largely unsuccessful.
To try and reveal why, researchers at the University of Michigan (U-M; Ann Arbor, USA) and Ecole Polytechnique (Palaiseau, France) developed a mathematical computer model that provided a three-dimensional (3D) image of exactly how SRT flowed through the lungs of patients in the three key trials that examined the technology. The first (1997) clinical study in adults showed promise, cutting mortality rate from 40% to 20%. But two larger studies in 2004 and 2011 showed no improvement in mortality, and the treatment was abandoned.
The computer model used fluid mechanical principals for 3-D modeling of the lung airway tree in both neonates and adults, showing how a liquid plug propagates through the tree from forced inspiration. In two separate modeling steps, they saw that the SRT plug deposits a coating film on the airway wall, and then splits unevenly at the bifurcation due to gravity. The model generates 3D images of the resulting acinar distribution and calculates two global indexes, efficiency and homogeneity.
When the researchers applied this engineering perspective to SRT, they saw one detail that set the successful 1997 study apart; a less concentrated version of medication was used. The SRT used in the 1997 study delivered the same dose of medication as the later studies, but it was dissolved in up to four times more liquid. The additional liquid helped the medication reach the tiny air sacs in the lungs. The study was published on July 13, 2015, in Proceedings of the National Academy of Sciences of the United States of America (PNAS).
“The medication needs to work its way from the trachea to tiny air sacs deep inside the lungs to be effective. This therapy is relatively straightforward in babies but more complex in adults, mostly because adult lungs are much bigger,” said lead author professor of biomedical engineering James Grotberg, MD, PhD, of the U-M College of Engineering. “The modeling technology could be used in other types of research as well, including more precise targeting of other medications in the lungs and projecting results from animal research to humans.”
Related Links:
University of Michigan
Ecole Polytechnique
Latest Critical Care News
- Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
- Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
- AI Model Could Help Diagnose Spinal Cord Disease Up To 30 Months Earlier
- 3D-Printed Swallowable Robot Could Perform Gastrointestinal Procedures
- Next-Gen Hydrogel Could Transform Soft Tissue and Organ Repair
- Engineered Cancer Eating Bacteria Consume Tumors from Inside Out
- ‘Cyborg’ Transplants Could Replace Pancreatic Tissue Damaged by Diabetes
- Smartphone-Linked Catheter Sensor Spots UTIs Sooner Than Lab Cultures
- AI Tool Identifies Trauma Patients Requiring Blood Transfusions Before Reaching Hospital
- New Clinical Guidelines to Reduce Central Line-Associated Bloodstream Infection
- New Inhalable Treatment for TB Lowers Side Effects
- AI Algorithm Improves Antibiotic Decision-Making in Urinary Tract Infection
- 3D-Printed System Enhances Vaccine Delivery Via Microneedle Array Patch
- Whole-Heart Mapping Technology Provides Comprehensive Real-Time View of Arrhythmias
- Wearable Device for Diabetics Could Replace Continuous Glucose Monitoring Systems
- AI Stethoscope Spots Heart Valve Disease Earlier Than GPs
Channels
Artificial Intelligence
view channelSurgical Techniques
view channel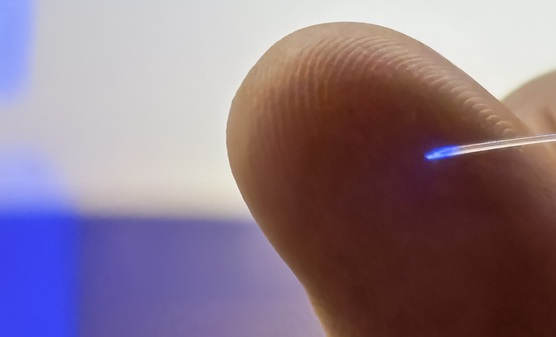
Brain Implant Records Neural Signals and Delivers Precise Medication
Neurological diseases such as epilepsy involve complex interactions across multiple layers of the brain, yet current implants can typically stimulate or record activity from only a single point.... Read moreAI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
Lipid-rich plaques inside coronary arteries are strongly associated with heart attacks and other major cardiac events. While optical coherence tomography (OCT) provides detailed images of vessel structure... Read moreNeural Device Regrows Surrounding Skull After Brain Implantation
Placing electronic implants on the brain typically requires removing a portion of the skull, creating challenges for long-term access and safe closure. Current methods often involve temporarily replacing the skull or securing metal plates, which can lead to complications such as skin erosion and additional surgeries.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more







.jpg)







