US Announces Agreement on Health Data Interoperability
|
By HospiMedica International staff writers Posted on 13 Mar 2016 |
The US Department of Health and Human Services (HHS; Washington DC, USA) has fostered an agreement on health data interoperability between providers and healthcare information technology (IT) firms.
More than a dozen leading professional associations and stakeholder groups pledged to implement three core commitments that will improve the flow of health information to consumers and healthcare providers. The first commitment is to help consumers easily and securely access their electronic health record (EHR) information, direct it to any desired location, learn how their information can be shared and used, and be assured that this information will be effectively and safely used to benefit their health and that of their community.
The second commitment is no information blocking by helping providers share personal EHR information with other providers and their patients whenever permitted by law, and not block EHR information, defined as knowingly and unreasonably interfering with information sharing.
The third commitment is to implement federally recognized, national interoperability standards, policies, guidance, and practices for electronic health information, and adopt best practices including those related to privacy and security. Many of the market leaders are embracing the Office of the National Coordinator for Health IT (ONC) Interoperability Standards Advisory, a coordinated catalog of existing and emerging standards and implementation specifications that is updated annually in order to keep pace with developments in the health IT industry.
“Today I am announcing that companies providing 90% of electronic health records used by hospitals have made a public commitment to make data work better for consumers and providers,” said Sylvia Burwell, secretary of the HHS, at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). “Consumer access remains a challenge; it's great to have an electronic record, but if that record can't be easily accessed by doctors and patients because of funky technology, then we aren't consistently seeing the benefit.”
“We commend HHS for bringing so many stakeholders together, all of whom have an interest in using technology to result in a healthier and more efficient health care system,” said Steven Stack, MD, president of the American Medical Association (AMA; Chicago, IL, USA). “Patients and physicians are in this effort together because patients need easy access to their electronic health information, confident that it is secure and can be shared to benefit their health, and physicians need these electronic records to be interoperable to ensure that patients are receiving the best care possible.”
Many of the biggest health IT developers have already committed to using standardized application programming interfaces and Health Level 7 (HL7) fast health care interoperability resources (FHIR), so that user-friendly devices, such as smartphone and tablet apps, can quickly be made market-ready and compatible with one another. The use of a single shared standard for communicating among devices will make it easier for consumers to access their test results, track progress in their care, and communicate with their providers.
Related Links:
US Department of Health and Human Services
American Medical Association
More than a dozen leading professional associations and stakeholder groups pledged to implement three core commitments that will improve the flow of health information to consumers and healthcare providers. The first commitment is to help consumers easily and securely access their electronic health record (EHR) information, direct it to any desired location, learn how their information can be shared and used, and be assured that this information will be effectively and safely used to benefit their health and that of their community.
The second commitment is no information blocking by helping providers share personal EHR information with other providers and their patients whenever permitted by law, and not block EHR information, defined as knowingly and unreasonably interfering with information sharing.
The third commitment is to implement federally recognized, national interoperability standards, policies, guidance, and practices for electronic health information, and adopt best practices including those related to privacy and security. Many of the market leaders are embracing the Office of the National Coordinator for Health IT (ONC) Interoperability Standards Advisory, a coordinated catalog of existing and emerging standards and implementation specifications that is updated annually in order to keep pace with developments in the health IT industry.
“Today I am announcing that companies providing 90% of electronic health records used by hospitals have made a public commitment to make data work better for consumers and providers,” said Sylvia Burwell, secretary of the HHS, at the annual meeting of the Healthcare Information and Management Systems Society (HIMSS). “Consumer access remains a challenge; it's great to have an electronic record, but if that record can't be easily accessed by doctors and patients because of funky technology, then we aren't consistently seeing the benefit.”
“We commend HHS for bringing so many stakeholders together, all of whom have an interest in using technology to result in a healthier and more efficient health care system,” said Steven Stack, MD, president of the American Medical Association (AMA; Chicago, IL, USA). “Patients and physicians are in this effort together because patients need easy access to their electronic health information, confident that it is secure and can be shared to benefit their health, and physicians need these electronic records to be interoperable to ensure that patients are receiving the best care possible.”
Many of the biggest health IT developers have already committed to using standardized application programming interfaces and Health Level 7 (HL7) fast health care interoperability resources (FHIR), so that user-friendly devices, such as smartphone and tablet apps, can quickly be made market-ready and compatible with one another. The use of a single shared standard for communicating among devices will make it easier for consumers to access their test results, track progress in their care, and communicate with their providers.
Related Links:
US Department of Health and Human Services
American Medical Association
Channels
Artificial Intelligence
view channelCritical Care
view channel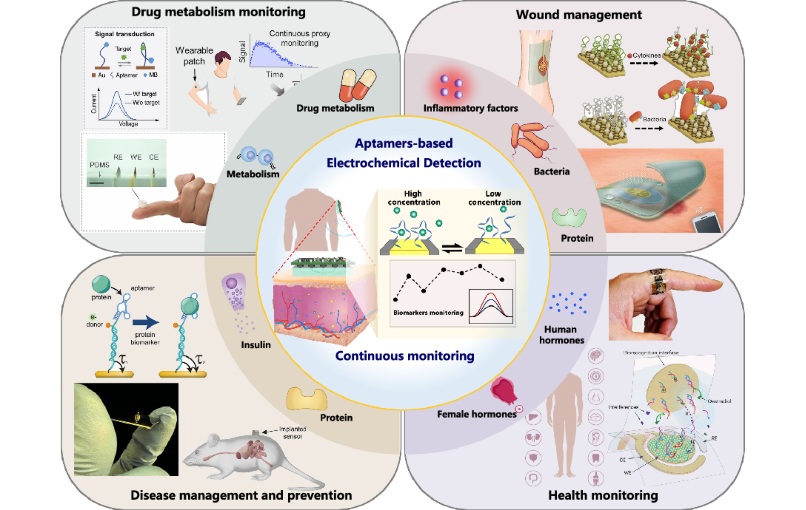
Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
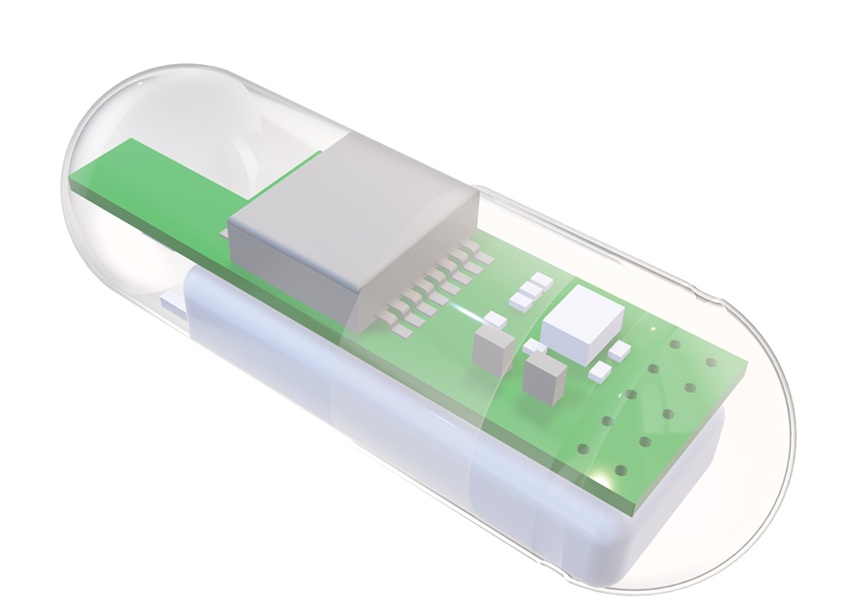
Continuous monitoring of biomarkers is critical for early disease detection, treatment evaluation, and personalized health management. Yet most clinical tests still rely on invasive, single-point blood... Read more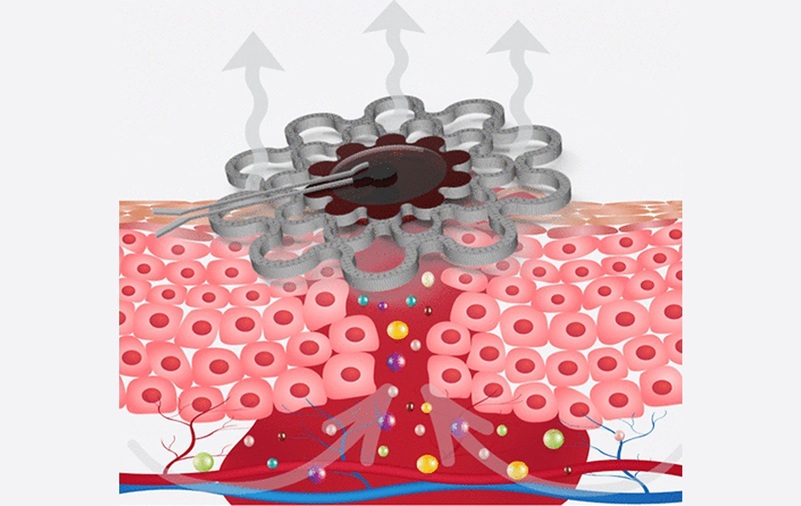
Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
Any wound has the potential to become chronic, but the risk is significantly higher in individuals with certain medical conditions. Once a wound becomes chronic, healing slows, complications increase,... Read moreSurgical Techniques
view channel
Redesigned Surgical Laser Cuts Bone Deeper and Faster Than Before
Lasers are valued in surgery for their precision and non-contact cutting, reducing mechanical stress and minimizing microcracks. While widely used for soft tissue, their application in hard tissues such... Read more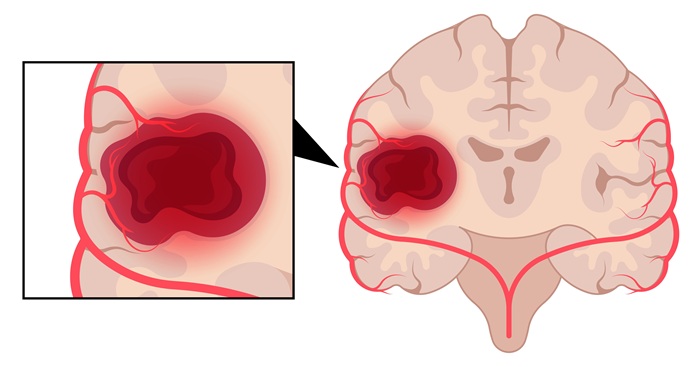
Laser Ablation Plus Immunotherapy Improves Survival in Recurrent Glioblastoma
Recurrent high-grade astrocytoma, including glioblastoma, is difficult to treat and often returns after surgery. Patients with recurrence typically survive only four to five months, highlighting a critical... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more