Lasers Help Breach Blood-Brain Barrier for Chemotherapy
|
By HospiMedica International staff writers Posted on 30 Mar 2016 |

Image: Neurosurgeon Eric Leuthardt, MD (Photo courtesy of WUSTL).
A new study reveals that laser beams can disrupt the blood-brain barrier (BBB) for up to six weeks, modifying its permeability long enough for chemotherapy treatment.
Researchers at Washington University School of Medicine (WUSTL; St. Louis, MO, USA) conducted a study involving 20 patients with probable recurrent glioblastoma to test a novel hyperthemic method designed to induce temporary disruption of the peritumoral BBB as a potential means to enhance drug delivery. The first step involves magnetic resonance imaging (MRI)-guided interstitial thermal therapy to create a 3-millimeter incision in the BBB, through which a neurosurgeon can robotically insert a laser to heat up and kill brain tumor cells.
To determine the degree and timing of peritumoral BBB disruption, dynamic contrast-enhanced brain MRI is used to calculate the vascular transfer constant (Ktrans) as a measure of permeability. The results showed that Ktrans levels in the peritumoral region peaked immediately post laser ablation, followed by a gradual decline over the following four weeks. Serum levels of brain-specific enolase (BSE), which were also measured and used as an independent quantification of BBB disruption, increased shortly after laser ablation, and peaked at 1-3 weeks before decreasing back to baseline by six weeks.
As part of the study, the chemotherapeutic agent doxorubicin was given intravenously to 13 patients in the weeks following the laser surgery. Preliminary data indicated that 12 of the patients showed no evidence of tumor progression during the 10-week time frame of the study. One patient experienced tumor growth before chemotherapy was delivered; the tumor in another patient progressed after chemotherapy was administered. Most patients went home after one to two days, and none experienced severe complications. The study was published on February 24, 2016, in PLOS One.
“The laser treatment kept the blood-brain barrier open for four to six weeks, providing us with a therapeutic window of opportunity to deliver chemotherapy drugs to the patients,” said lead author Professor of neurosurgery Eric Leuthardt, MD. “This is crucial because most chemotherapy drugs can’t get past the protective barrier, greatly limiting treatment options for patients with brain tumors.”
The BBB is comprised of specialized endothelial cells that form the capillary microvasculature of the central nervous system (CNS), and is essential for brain function. It selectively prevents substances from entering the blood and brain, only allowing such essential molecules as amino acids, oxygen, glucose and water through. On the other hand, it also poses the greatest impediment in the treatment of many CNS diseases because it commonly blocks entry of therapeutic compounds.
Related Links:
Washington University School of Medicine
Researchers at Washington University School of Medicine (WUSTL; St. Louis, MO, USA) conducted a study involving 20 patients with probable recurrent glioblastoma to test a novel hyperthemic method designed to induce temporary disruption of the peritumoral BBB as a potential means to enhance drug delivery. The first step involves magnetic resonance imaging (MRI)-guided interstitial thermal therapy to create a 3-millimeter incision in the BBB, through which a neurosurgeon can robotically insert a laser to heat up and kill brain tumor cells.
To determine the degree and timing of peritumoral BBB disruption, dynamic contrast-enhanced brain MRI is used to calculate the vascular transfer constant (Ktrans) as a measure of permeability. The results showed that Ktrans levels in the peritumoral region peaked immediately post laser ablation, followed by a gradual decline over the following four weeks. Serum levels of brain-specific enolase (BSE), which were also measured and used as an independent quantification of BBB disruption, increased shortly after laser ablation, and peaked at 1-3 weeks before decreasing back to baseline by six weeks.
As part of the study, the chemotherapeutic agent doxorubicin was given intravenously to 13 patients in the weeks following the laser surgery. Preliminary data indicated that 12 of the patients showed no evidence of tumor progression during the 10-week time frame of the study. One patient experienced tumor growth before chemotherapy was delivered; the tumor in another patient progressed after chemotherapy was administered. Most patients went home after one to two days, and none experienced severe complications. The study was published on February 24, 2016, in PLOS One.
“The laser treatment kept the blood-brain barrier open for four to six weeks, providing us with a therapeutic window of opportunity to deliver chemotherapy drugs to the patients,” said lead author Professor of neurosurgery Eric Leuthardt, MD. “This is crucial because most chemotherapy drugs can’t get past the protective barrier, greatly limiting treatment options for patients with brain tumors.”
The BBB is comprised of specialized endothelial cells that form the capillary microvasculature of the central nervous system (CNS), and is essential for brain function. It selectively prevents substances from entering the blood and brain, only allowing such essential molecules as amino acids, oxygen, glucose and water through. On the other hand, it also poses the greatest impediment in the treatment of many CNS diseases because it commonly blocks entry of therapeutic compounds.
Related Links:
Washington University School of Medicine
Latest Surgical Techniques News
- Novel Endoscopy Technique Provides Access to Deep Lung Tumors
- New Study Findings Could Halve Number of Stent Procedures
- Breakthrough Surgical Device Redefines Hip Arthroscopy
- Automated System Enables Real-Time "Molecular Pathology" During Cancer Surgery
- Groundbreaking Procedure Combines New Treatments for Liver Tumors
- Ablation Reduces Stroke Risk Associated with Atrial Fibrillation
- Optical Tracking Method Identifies Target Areas in Robot-Assisted Neurosurgery
- General Anesthesia Improves Post-Surgery Outcomes for Acute Stroke Patients
- Drug-Coated Balloons Can Replace Stents Even in Larger Coronary Arteries
- Magnetic Kidney Stone Retrieval Device Outperforms Ureteroscopic Laser Lithotripsy
- Absorbable Skull Device Could Replace Traditional Metal Implants Used After Brain Surgery
- Magic Silicone Liquid Powered Robots Perform MIS in Narrow Cavities
- 'Lab-on-a-Scalpel' Provides Real-Time Surgical Insights for POC Diagnostics in OR
- Biodegradable Brain Implant Prevents Glioblastoma Recurrence
- Tiny 3D Printer Reconstructs Tissues During Vocal Cord Surgery
- Minimally Invasive Procedure for Aortic Valve Disease Has Similar Outcomes as Surgery
Channels
Critical Care
view channel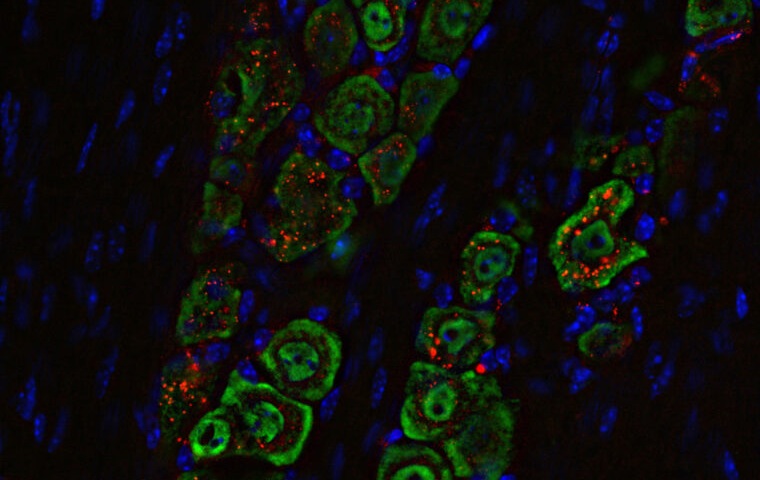
Nasal Drops Fight Brain Tumors Noninvasively
Glioblastoma is one of the most aggressive and fatal brain cancers, progressing rapidly and leaving patients with very limited treatment options. A major challenge has been delivering effective therapies... Read more
AI Helps Optimize Therapy Selection and Dosing for Septic Shock
Septic shock is a life-threatening complication of sepsis and remains a leading cause of hospital deaths worldwide. Patients experience dangerously low blood pressure that can rapidly lead to organ failure,... Read more
Glowing Bacteria ‘Pills’ for Detecting Gut Diseases Could Eliminate Colonoscopies
Diagnosing gastrointestinal diseases such as colitis and colorectal cancer often relies on colonoscopy, an invasive procedure that many patients avoid despite ongoing symptoms like bleeding, cramping, and diarrhoea.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more