LVAD Survival Better When Combined with ICD
|
By HospiMedica International staff writers Posted on 19 Jul 2016 |
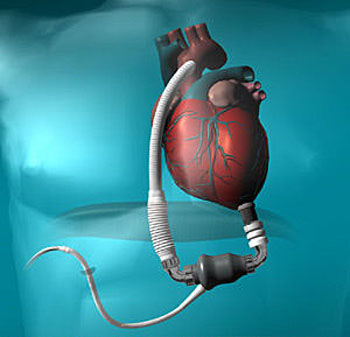
Image: According to a new study, patient survival with a left ventricular assist device (LVAD) is better when an implantable cardioverter defibrillator (ICD) is also present (Photo courtesy of BCM).
Researchers at the Minneapolis Veterans Affairs (VA) Health Care System (MN, USA) conducted a systematic review and meta-analysis of studies published in PubMed and OVID databases from January 2000 through October 2015 in order to evaluate the impact of ICDs on mortality in patients with LVADs. In all, six relevant studies were identified, which included 937 patients (mean age 53 years, 80% male). A continuous-flow LVAD was present in 39% of the patients, and an ICD was present in 38%.
The results showed that among LVAD patients, all-cause mortality rates were 16% with an ICD, versus 32% without one, over a mean follow-up period of 7 months. Patients with newer, continuous flow LVADs showed a similar, but non-significant trend for better survival with an ICD (14% versus 25%, respectively). The authors acknowledged that they failed to totally exclude patients with biventricular assist devices (17%) and right ventricular assist devices (4%). The study was published in the July 2016 issue of JACC: Heart Failure.
“The evidence supporting ICD use in patients with LVADs is limited to a few, relatively small studies. Current practice guidelines supporting ICD use in LVAD patients are therefore predominantly based on expert consensus and observational studies,” wrote lead author Kairav Vakil, MD, and colleagues, adding that, “this cohort was enriched with patients that received an LVAD as bridge-to-transplantation. As such, these results cannot be generalized to patients receiving destination therapy LVADs, who are known to be relatively sicker than those awaiting transplantation.”
An LVAD is intended to complement a weakened heart by providing circulatory support. Surgically implanted in proximity to the heart, one end is attached to the left ventricle, while the other is attached to the aorta. Blood flows from the ventricles into the pump and is then ejected out of the device and into the aorta. Although the mechanism of survival benefit from ICDs in LVAD patients remains unclear, a possible explanation is that it may contribute to a reduction in harmful effects of ventricular arrhythmias on right ventricular function, thereby leading to reduction of heart failure deaths.
Related Links:
Minneapolis Veterans Affairs
The results showed that among LVAD patients, all-cause mortality rates were 16% with an ICD, versus 32% without one, over a mean follow-up period of 7 months. Patients with newer, continuous flow LVADs showed a similar, but non-significant trend for better survival with an ICD (14% versus 25%, respectively). The authors acknowledged that they failed to totally exclude patients with biventricular assist devices (17%) and right ventricular assist devices (4%). The study was published in the July 2016 issue of JACC: Heart Failure.
“The evidence supporting ICD use in patients with LVADs is limited to a few, relatively small studies. Current practice guidelines supporting ICD use in LVAD patients are therefore predominantly based on expert consensus and observational studies,” wrote lead author Kairav Vakil, MD, and colleagues, adding that, “this cohort was enriched with patients that received an LVAD as bridge-to-transplantation. As such, these results cannot be generalized to patients receiving destination therapy LVADs, who are known to be relatively sicker than those awaiting transplantation.”
An LVAD is intended to complement a weakened heart by providing circulatory support. Surgically implanted in proximity to the heart, one end is attached to the left ventricle, while the other is attached to the aorta. Blood flows from the ventricles into the pump and is then ejected out of the device and into the aorta. Although the mechanism of survival benefit from ICDs in LVAD patients remains unclear, a possible explanation is that it may contribute to a reduction in harmful effects of ventricular arrhythmias on right ventricular function, thereby leading to reduction of heart failure deaths.
Related Links:
Minneapolis Veterans Affairs
Latest Critical Care News
- 3D-Printed Swallowable Robot Could Perform Gastrointestinal Procedures
- Next-Gen Hydrogel Could Transform Soft Tissue and Organ Repair
- Engineered Cancer Eating Bacteria Consume Tumors from Inside Out
- ‘Cyborg’ Transplants Could Replace Pancreatic Tissue Damaged by Diabetes
- Smartphone-Linked Catheter Sensor Spots UTIs Sooner Than Lab Cultures
- AI Tool Identifies Trauma Patients Requiring Blood Transfusions Before Reaching Hospital
- New Clinical Guidelines to Reduce Central Line-Associated Bloodstream Infection
- New Inhalable Treatment for TB Lowers Side Effects
- AI Algorithm Improves Antibiotic Decision-Making in Urinary Tract Infection
- 3D-Printed System Enhances Vaccine Delivery Via Microneedle Array Patch
- Whole-Heart Mapping Technology Provides Comprehensive Real-Time View of Arrhythmias
- Wearable Device for Diabetics Could Replace Continuous Glucose Monitoring Systems
- AI Stethoscope Spots Heart Valve Disease Earlier Than GPs
- Bioadhesive Patch Eliminates Cancer Cells That Remain After Brain Tumor Surgery
- Wearable Patch Provides Up-To-The-Minute Readouts of Medication Levels in Body
- New Spray-Mist Device Delivers Antibiotics Directly into Infected Tissue
Channels
Artificial Intelligence
view channelSurgical Techniques
view channelAI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
Lipid-rich plaques inside coronary arteries are strongly associated with heart attacks and other major cardiac events. While optical coherence tomography (OCT) provides detailed images of vessel structure... Read moreNeural Device Regrows Surrounding Skull After Brain Implantation
Placing electronic implants on the brain typically requires removing a portion of the skull, creating challenges for long-term access and safe closure. Current methods often involve temporarily replacing the skull or securing metal plates, which can lead to complications such as skin erosion and additional surgeries.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more
















