Vital Sign Volatility on Discharge Quadruples Mortality Risk
|
By HospiMedica International staff writers Posted on 25 Aug 2016 |

Image: Dr. Oanh Nguyen (left), Dr. Anil Makam (center), and Dr. Ethan A. Halm (right). A new study reveals that 20% of people are released from hospital before all vital signs are stable, and subsequently face a significantly higher risk of post-discharge adverse outcomes (Photo courtesy of UT Southwestern’s Center for Patient-Centered Outcomes Research).
Researchers at the University of Texas (UT) Southwestern Medical Centre (Dallas, TX, USA) reviewed the electronic medical records (EMR) of 32,835 unique individuals from six Dallas-Fort Worth area hospitals to assess the association between vital sign instability at hospital discharge and post-discharge outcomes, including abnormalities in temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation within 24 hours of discharge. Main measures included death or non-elective readmission within 30 days.
The results showed that 18.7% of the patients were discharged with one or more vital sign instabilities. And while 12.8% of individuals with no instabilities on discharge died or were readmitted, patients with one instability demonstrated a 16.9% tendency for adverse events, those with two instabilities showed a 21.2% tendency, and patients with three or more instabilities died or were readmitted 26% of the time. The presence of any instability was associated with higher risk-adjusted odds of either death or readmission, and was more strongly associated with death.
Patients with three or more instabilities had nearly four-fold increased odds of death and 40% increased odds of 30-day readmission compared to those with no instabilities. Analysis using logistic regression adjusted for predictors of 30-day death and readmission showed that having two or more vital sign instabilities at discharge had a positive predictive value of 22 % and positive likelihood ratio of 1.8 for 30-day death or readmission. The study was published on August 8, 2016, in Journal of General Internal Medicine.
“We found that nearly 1 in 5 hospitalized adults is discharged with one or more vital sign instabilities such as an elevated heart rate or low blood pressure,” said lead author Oanh Nguyen, MD, and assistant professor of internal medicine and clinical sciences. “This finding is an important patient safety issue because patients who had vital sign abnormalities on the day of discharge had higher rates of hospital readmission and death within 30 days, even after adjusting for many other risk factors.”
“At a time when people are developing complicated, black box computerized algorithms to identify patients at high risk of readmission, our study highlights that the stability of vital signs, something doctors review with their own eyes every day, is a simple, clinically objective means of assessing readiness and safety for discharge,” said senior author Ethan Halm, MD, director of the UT Southwestern Center for Patient-Centered Outcomes Research. “There's a good reason we call them vital signs. It is important for clinicians to look at all of the vital signs in the 24 hours prior to discharge, and not just the last set or the best ones in judging a patient's readiness for discharge.”
Related Links:
University of Texas (UT) Southwestern Medical Centre
The results showed that 18.7% of the patients were discharged with one or more vital sign instabilities. And while 12.8% of individuals with no instabilities on discharge died or were readmitted, patients with one instability demonstrated a 16.9% tendency for adverse events, those with two instabilities showed a 21.2% tendency, and patients with three or more instabilities died or were readmitted 26% of the time. The presence of any instability was associated with higher risk-adjusted odds of either death or readmission, and was more strongly associated with death.
Patients with three or more instabilities had nearly four-fold increased odds of death and 40% increased odds of 30-day readmission compared to those with no instabilities. Analysis using logistic regression adjusted for predictors of 30-day death and readmission showed that having two or more vital sign instabilities at discharge had a positive predictive value of 22 % and positive likelihood ratio of 1.8 for 30-day death or readmission. The study was published on August 8, 2016, in Journal of General Internal Medicine.
“We found that nearly 1 in 5 hospitalized adults is discharged with one or more vital sign instabilities such as an elevated heart rate or low blood pressure,” said lead author Oanh Nguyen, MD, and assistant professor of internal medicine and clinical sciences. “This finding is an important patient safety issue because patients who had vital sign abnormalities on the day of discharge had higher rates of hospital readmission and death within 30 days, even after adjusting for many other risk factors.”
“At a time when people are developing complicated, black box computerized algorithms to identify patients at high risk of readmission, our study highlights that the stability of vital signs, something doctors review with their own eyes every day, is a simple, clinically objective means of assessing readiness and safety for discharge,” said senior author Ethan Halm, MD, director of the UT Southwestern Center for Patient-Centered Outcomes Research. “There's a good reason we call them vital signs. It is important for clinicians to look at all of the vital signs in the 24 hours prior to discharge, and not just the last set or the best ones in judging a patient's readiness for discharge.”
Related Links:
University of Texas (UT) Southwestern Medical Centre
Latest Critical Care News
- AI-Enhanced Echocardiography Improves Early Detection of Amyloid Buildup in Heart
- Consumer Wearables Could Predict Pediatric Surgery Complications
- Wireless Implant Delivers Chemotherapy Deep into Tumors Without Side Effects
- Skin-Like Sensor Monitors Vital Signs and Tracks Healing After Surgery
- Implantable Device Could Save Diabetes Patients from Dangerously Low Blood Sugar
- New Prostate Screening Device Could Replace Traditional Examination Method
- Adaptive Spine Board to Revolutionize ER Transport
- Mapping Communication Between Internal Organs to Enable Earlier Illness Diagnosis
- Intelligent Wound Dressing Reduces Inflammation and Promotes Healing
- Cuff-Free Blood Pressure Monitoring Device to Improve Early Detection and Management of Hypertension
- New Understanding of Barrett’s Esophagus Formation to Enable Earlier Intervention and Diagnosis
- 3D Printed Functional Human Islets Could Transform Type 1 Diabetes Treatment
- AI Model Predicts ICU mortality in Heart Failure Patients
- Smart Capsule Offers Real-Time Profiling Across GI Tract
- Ultra-Thin Implant Helps Patients with Spinal Cord Injury Recover Lost Functions
- Portable Cell Therapy Device to Enable Rapid On-Demand Modification of RBCs at POC
Channels
Surgical Techniques
view channel
Fluorescent Imaging Agent ‘Lights Up’ Nerves for Better Visualization During Surgery
Surgical nerve injury is a significant concern in head and neck surgeries, where nerves are at risk of being inadvertently damaged during procedures. Such injuries can lead to complications that may impact... Read more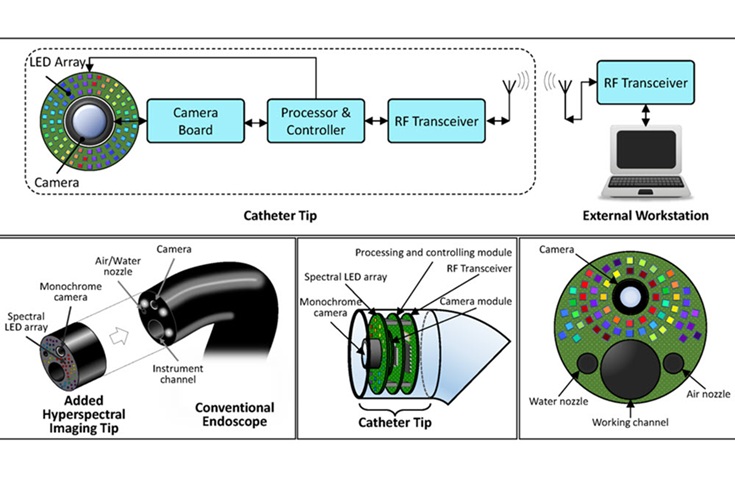
LED-Based Imaging System Could Transform Cancer Detection in Endoscopy
Gastrointestinal cancers remain one of the most common and challenging forms of cancer to diagnose accurately. Despite the widespread use of endoscopy for screening and diagnosis, the procedure still misses... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
A research collaboration will focus on the joint discovery of novel therapeutic approaches based on findings in human genomics research related to cardiovascular diseases. Bayer (Berlin, Germany) and... Read more