New Treatment Option for Failing Pulmonary Valve Conduits
|
By HospiMedica International staff writers Posted on 04 Apr 2017 |

Image: The Melody TPV can now serve as a bridge for surgery (Photo courtesy of Medtronic).
A novel transcatheter pulmonary valve (TPV) can now offer a minimally invasive solution for patients whose surgical bioprosthetic pulmonary heart valves have failed.
The Medtronic Melody TPV is specifically designed to treat patients with right ventricular outflow tract (RVOT) valve dysfunction resulting from congenital heart disease (CHD). It is comprised of a bovine jugular vein (BJV) valve that is sutured within a platinum iridium frame, which provides natural venous valve leaflets that open and close under minimal pressure, resulting in optimal hemodynamics. The deep coaptation of the leaflets also provides valve competency across a range of conduit sizes and geometries.
Melody TPV placement is via a transcatheter procedure using the Medtronic Ensemble delivery system under fluoroscopic guidance, using balloon-in-balloon (BIB) technology for controlled deployment of the valve, which includes a radiopaque stent for visualization ease during the procedure. In addition to the initial indication for the Melody TPV to prolong the time between open-heart surgeries for patients with a pulmonary conduit caused by CHD, it can now be also used to replace a failed surgical bioprosthetic pulmonary heart valve as an interim solution to further surgery.
“Unlike other transcatheter valves currently on the market, Melody TPV is uniquely designed for use in the pulmonic position, and is thus well suited for implantation in failed surgical pulmonary heart valves,” said Rhonda Robb, vice president and general manager of the heart valve therapies business unit at Medtronic. “This approval further demonstrates our commitment to improving treatment options for congenital heart disease and we look forward to bringing this proven non-surgical option to congenital patients.”
“The Melody TPV brought a breakthrough non-surgical option to treat failing pulmonary valve conduits; thousands of congenital patients globally have benefited from this therapy in the past decade,” said Jeremy Asnes, MD, associate director of the congenital cardiac catheterization laboratory at Yale School of Medicine (New Haven, CT, USA). “With this expanded indication, we can further reduce the need for obtrusive open-heart surgery, and allow even more patients to benefit from this minimally invasive treatment option.”
Surgical correction of CHD defects such as Tetralogy of Fallot and pulmonary atresia has increased dramatically over the last several decades. But despite excellent long-term survival, they typically require multiple operative procedures until adulthood, as the homograft pulmonary artery conduits or BJV grafts have no ability to grow and remodel with the somatic growth of the child. Additionally, an intense inflammatory reaction to these materials commonly occurs, resulting in early calcification and failure, leading typically to the need for 5-7 operative procedures during the patient’s lifetime.
The Medtronic Melody TPV is specifically designed to treat patients with right ventricular outflow tract (RVOT) valve dysfunction resulting from congenital heart disease (CHD). It is comprised of a bovine jugular vein (BJV) valve that is sutured within a platinum iridium frame, which provides natural venous valve leaflets that open and close under minimal pressure, resulting in optimal hemodynamics. The deep coaptation of the leaflets also provides valve competency across a range of conduit sizes and geometries.
Melody TPV placement is via a transcatheter procedure using the Medtronic Ensemble delivery system under fluoroscopic guidance, using balloon-in-balloon (BIB) technology for controlled deployment of the valve, which includes a radiopaque stent for visualization ease during the procedure. In addition to the initial indication for the Melody TPV to prolong the time between open-heart surgeries for patients with a pulmonary conduit caused by CHD, it can now be also used to replace a failed surgical bioprosthetic pulmonary heart valve as an interim solution to further surgery.
“Unlike other transcatheter valves currently on the market, Melody TPV is uniquely designed for use in the pulmonic position, and is thus well suited for implantation in failed surgical pulmonary heart valves,” said Rhonda Robb, vice president and general manager of the heart valve therapies business unit at Medtronic. “This approval further demonstrates our commitment to improving treatment options for congenital heart disease and we look forward to bringing this proven non-surgical option to congenital patients.”
“The Melody TPV brought a breakthrough non-surgical option to treat failing pulmonary valve conduits; thousands of congenital patients globally have benefited from this therapy in the past decade,” said Jeremy Asnes, MD, associate director of the congenital cardiac catheterization laboratory at Yale School of Medicine (New Haven, CT, USA). “With this expanded indication, we can further reduce the need for obtrusive open-heart surgery, and allow even more patients to benefit from this minimally invasive treatment option.”
Surgical correction of CHD defects such as Tetralogy of Fallot and pulmonary atresia has increased dramatically over the last several decades. But despite excellent long-term survival, they typically require multiple operative procedures until adulthood, as the homograft pulmonary artery conduits or BJV grafts have no ability to grow and remodel with the somatic growth of the child. Additionally, an intense inflammatory reaction to these materials commonly occurs, resulting in early calcification and failure, leading typically to the need for 5-7 operative procedures during the patient’s lifetime.
Latest Surgical Techniques News
- NIR Light Enables Powering and Communicating with Implantable Medical Devices
- Simple Bypass Protocol Improves Outcomes in Chronic Cerebral Occlusion
- Implantable Absorbable Sensor Detects Life-Threatening Complications After Intestinal Surgery
- New Study Findings Enable Improved Ventilation During Complex Lung Surgery
- 3D-Printed Blood Vessel Scaffolds Could Transform Heart Bypass Surgeries
- Novel Imaging Technique Helps View Blood Perfusion During Esophageal Surgery
- Minimally Invasive Surgery Proven Safe and Effective for Complex ‘Whipple’ Procedure
- Catheter-Based Procedures Offer Less Invasive Option for Treatment of Valvular Disease
- Laparoscopic Surgery Improves Outcomes for Severe Newborn Liver Disease
- Novel Endoscopy Technique Provides Access to Deep Lung Tumors
- New Study Findings Could Halve Number of Stent Procedures
- Breakthrough Surgical Device Redefines Hip Arthroscopy
- Automated System Enables Real-Time "Molecular Pathology" During Cancer Surgery
- Groundbreaking Procedure Combines New Treatments for Liver Tumors
- Ablation Reduces Stroke Risk Associated with Atrial Fibrillation
- Optical Tracking Method Identifies Target Areas in Robot-Assisted Neurosurgery
Channels
Critical Care
view channel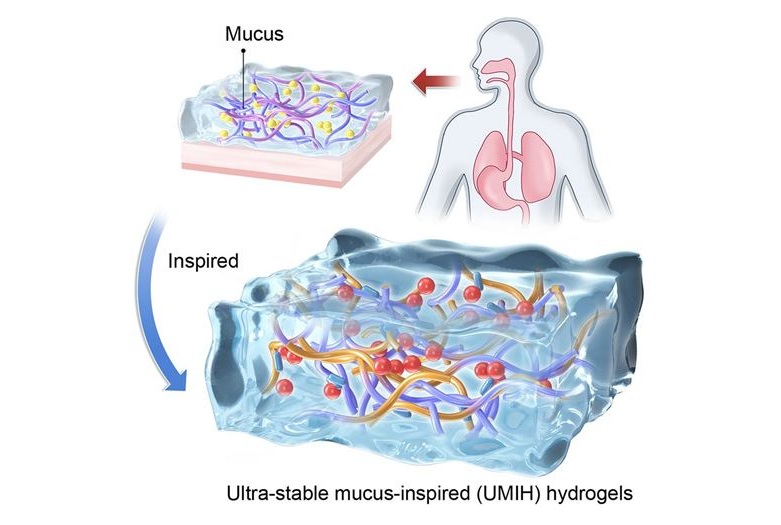
Ultra-Stable Mucus-Inspired Hydrogel Boosts Gastrointestinal Wound Healing
Treating wounds and delivering drugs in the gastrointestinal tract is challenging because most biomaterials rapidly degrade in the stomach’s highly acidic environment. Conventional hydrogels lose adhesion... Read more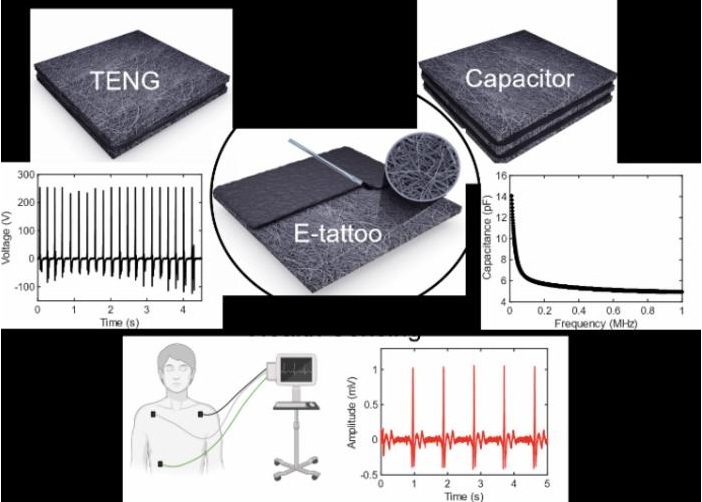
E-Tattoos Harvest Energy and Monitor Health in Real Time
Wearable health devices are increasingly used for continuous monitoring, but many rely on rigid components, external gels, or frequent battery charging, limiting comfort and long-term use.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more