CLND Fails to Improve Melanoma Survival Rates
|
By HospiMedica International staff writers Posted on 19 Jun 2017 |
A new study shows that immediate completion lymph-node dissection (CLND) does not increase survival among patients with melanoma and sentinel-node metastases.
Researchers at the John Wayne Cancer Institute (JWCI; Santa Monica, CA, USA), Sentara CarePlex Hospital (Hampton, VA, USA), and other institutions worldwide conducted a study that randomly assigned 1,934 patients with sentinel-node metastases--detected via standard pathological assessment or a multimarker molecular assay--to immediate CLND or to an observation group monitored with ultrasonography. Main outcomes and measures were melanoma-specific survival, disease-free survival, and cumulative rate of non-sentinel-node metastasis.
The results showed that Immediate CLND was not associated with increased melanoma-specific survival. In the per-protocol analysis, the mean three-year rate of melanoma-specific survival was similar in the dissection group and the observation group (86%) at a median follow-up of 43 months. The mean rate of disease-free survival was slightly higher in the dissection group (68%) than in the observation group (63%) at three years. Lymphedema was observed in 24.1% of the patients in the dissection group and in 6.3% of those in the observation group. The study was published on June 8, 2017, in the New England Journal of Medicine (NEJM).
“Although the completion dissections did not help overall survival, they did have some value. By examining the dissected lymph nodes, physicians were able to better gauge how extensively the cancer had spread and to lengthen the time that their patients were disease-free. But those advantages did not translate into longer lives,” said lead author Mark Faries, MD, of JWCI. “The new findings likely will result in many fewer of these procedures being performed around the world. The results also will likely affect the design of many current and future clinical trials of medical therapies in melanoma.”
Lymph nodes, located throughout the body, serve as biologic filters that contain immune cells that fight infection and clean the blood. When cancer cells break away from a tumor, the cells can travel through the lymph system; sentinel node surgery allows the surgeon to remove the nodes to determine cancer spread. As human nodes are only 5 mm in size, they are difficult to discern from the surrounding tissue during surgery. Furthermore, even when surgeons are able to map the location of the nodes, there is no current technique that indicates whether or not the lymph nodes contain cancer, requiring removal of more lymph nodes than necessary.
Related Links:
John Wayne Cancer Institute
Sentara CarePlex Hospital
Researchers at the John Wayne Cancer Institute (JWCI; Santa Monica, CA, USA), Sentara CarePlex Hospital (Hampton, VA, USA), and other institutions worldwide conducted a study that randomly assigned 1,934 patients with sentinel-node metastases--detected via standard pathological assessment or a multimarker molecular assay--to immediate CLND or to an observation group monitored with ultrasonography. Main outcomes and measures were melanoma-specific survival, disease-free survival, and cumulative rate of non-sentinel-node metastasis.
The results showed that Immediate CLND was not associated with increased melanoma-specific survival. In the per-protocol analysis, the mean three-year rate of melanoma-specific survival was similar in the dissection group and the observation group (86%) at a median follow-up of 43 months. The mean rate of disease-free survival was slightly higher in the dissection group (68%) than in the observation group (63%) at three years. Lymphedema was observed in 24.1% of the patients in the dissection group and in 6.3% of those in the observation group. The study was published on June 8, 2017, in the New England Journal of Medicine (NEJM).
“Although the completion dissections did not help overall survival, they did have some value. By examining the dissected lymph nodes, physicians were able to better gauge how extensively the cancer had spread and to lengthen the time that their patients were disease-free. But those advantages did not translate into longer lives,” said lead author Mark Faries, MD, of JWCI. “The new findings likely will result in many fewer of these procedures being performed around the world. The results also will likely affect the design of many current and future clinical trials of medical therapies in melanoma.”
Lymph nodes, located throughout the body, serve as biologic filters that contain immune cells that fight infection and clean the blood. When cancer cells break away from a tumor, the cells can travel through the lymph system; sentinel node surgery allows the surgeon to remove the nodes to determine cancer spread. As human nodes are only 5 mm in size, they are difficult to discern from the surrounding tissue during surgery. Furthermore, even when surgeons are able to map the location of the nodes, there is no current technique that indicates whether or not the lymph nodes contain cancer, requiring removal of more lymph nodes than necessary.
Related Links:
John Wayne Cancer Institute
Sentara CarePlex Hospital
Latest Surgical Techniques News
- AI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
- Neural Device Regrows Surrounding Skull After Brain Implantation
- Surgical Innovation Cuts Ovarian Cancer Risk by 80%
- New Imaging Combo Offers Hope for High-Risk Heart Patients
- New Classification System Brings Clarity to Brain Tumor Surgery Decisions
- Boengineered Tissue Offers New Hope for Secondary Lymphedema Treatment
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- New AI Approach to Improve Surgical Imaging
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- Ultrasound Device Offers Non-Invasive Treatment for Kidney Stones
- Light-Activated Tissue Adhesive Patch Achieves Rapid and Watertight Neurosurgical Sealing
- Minimally Invasive Coronary Artery Bypass Method Offers Safer Alternative to Open-Heart Surgery
- Injectable Breast ‘Implant’ Offers Alternative to Traditional Surgeries
- AI Detects Stomach Cancer Risk from Upper Endoscopic Images
- NIR Light Enables Powering and Communicating with Implantable Medical Devices
Channels
Artificial Intelligence
view channelCritical Care
view channel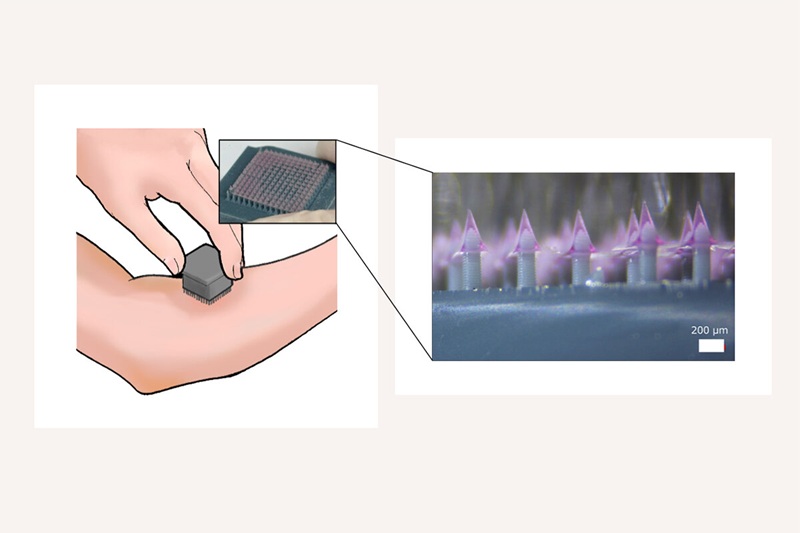
3D-Printed Delivery System Enhances Vaccine Delivery Via Microneedle Array Patch
The COVID-19 pandemic underscored the need for efficient, durable, and widely accessible vaccines. Conventional vaccination requires trained personnel and cold-chain logistics, which can slow mass immunization... Read more
Whole-Heart Mapping Technology Provides Comprehensive Real-Time View of Arrhythmias
Cardiac arrhythmias can be difficult to diagnose and treat because current mapping systems analyze the heart one chamber at a time. This fragmented view forces clinicians to infer electrical activity they... Read more
Wearable Device for Diabetics Could Replace Continuous Glucose Monitoring Systems
Monitoring blood glucose is essential for people with diabetes to prevent complications and maintain long-term health. Current continuous glucose monitoring systems require needles inserted under the skin,... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more







.jpg)







