Blood Management Program Reduces Unnecessary Transfusions
|
By HospiMedica International staff writers Posted on 26 Sep 2017 |

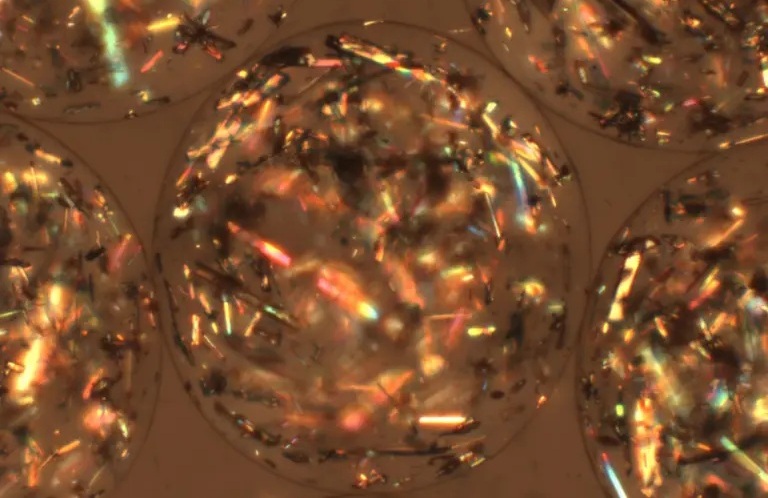
Image: A new study claims a program to reduce unnecessary blood transfusions has improved patient care (Photo courtesy of Keith Weller / JHU).
Implementing a system-wide patient blood management program (BMP) can substantially reduce blood utilization and blood acquisition costs, claims a new study.
The blood management clinical community, formed at Johns Hopkins University School of Medicine (JHU-SOM; Baltimore, MD, USA), is a physician-led, multidisciplinary, collaborative, quality-improvement team formed in order to implement best practices for patient blood management. To determine the effectiveness of the system, changes in blood utilization and blood acquisition costs were compared for the pre- and post-patient BMP implementation time periods.
The results revealed that across the health system, multiunit erythrocyte transfusion orders decreased from 39.7% to 20.2%, almost half. The percentage of patients transfused decreased for erythrocytes from 11.3% to 10.4%, for plasma from 2.9% to 2.2%, and for platelets from 3.1% to 2.7%. The number of units transfused per 1,000 patients also decreased; for erythrocytes by 19.8%; for plasma by 38.9%; and for platelets by 15.6%. Overall blood acquisition cost savings were USD 2,120,273 per year, an estimated 400% return on investment. The study was published on September 7, 2017, in Anesthesiology.
“Hospitals across the country are merging into health systems, in part to realize economies of scale by improving quality. Our experience with a patient blood management program shows that it's feasible to do that,” said lead author professor of anesthesiology and critical care medicine Steven Frank, MD. “Our premise is that doctors don't want to be told how to practice medicine by computer pop-up alerts; they would rather hear about the studies supporting the guidelines.”
The PBM program was launched in January 2012 at the Johns Hopkins Hospital with a clinical education program that consisted of live, in-person grand rounds presentations to various clinical departments in order to inform physicians, nurses, and other staff about hospital transfusion policy guidelines, and the results of eight published landmark studies that support reduced use of transfusions. The single most effective intervention, according to the study, was the “Why give 2 when 1 will do?" campaign to encourage single-unit transfusions.
Related Links:
Johns Hopkins University School of Medicine
The blood management clinical community, formed at Johns Hopkins University School of Medicine (JHU-SOM; Baltimore, MD, USA), is a physician-led, multidisciplinary, collaborative, quality-improvement team formed in order to implement best practices for patient blood management. To determine the effectiveness of the system, changes in blood utilization and blood acquisition costs were compared for the pre- and post-patient BMP implementation time periods.
The results revealed that across the health system, multiunit erythrocyte transfusion orders decreased from 39.7% to 20.2%, almost half. The percentage of patients transfused decreased for erythrocytes from 11.3% to 10.4%, for plasma from 2.9% to 2.2%, and for platelets from 3.1% to 2.7%. The number of units transfused per 1,000 patients also decreased; for erythrocytes by 19.8%; for plasma by 38.9%; and for platelets by 15.6%. Overall blood acquisition cost savings were USD 2,120,273 per year, an estimated 400% return on investment. The study was published on September 7, 2017, in Anesthesiology.
“Hospitals across the country are merging into health systems, in part to realize economies of scale by improving quality. Our experience with a patient blood management program shows that it's feasible to do that,” said lead author professor of anesthesiology and critical care medicine Steven Frank, MD. “Our premise is that doctors don't want to be told how to practice medicine by computer pop-up alerts; they would rather hear about the studies supporting the guidelines.”
The PBM program was launched in January 2012 at the Johns Hopkins Hospital with a clinical education program that consisted of live, in-person grand rounds presentations to various clinical departments in order to inform physicians, nurses, and other staff about hospital transfusion policy guidelines, and the results of eight published landmark studies that support reduced use of transfusions. The single most effective intervention, according to the study, was the “Why give 2 when 1 will do?" campaign to encourage single-unit transfusions.
Related Links:
Johns Hopkins University School of Medicine
Latest Surgical Techniques News
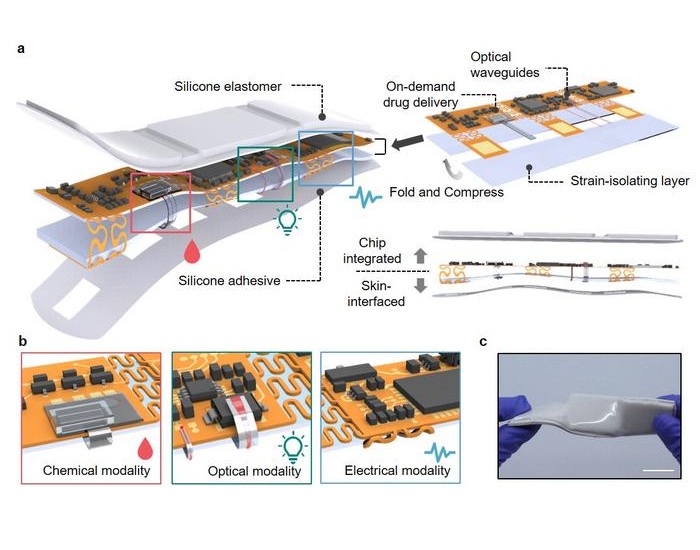
- Neural Device Regrows Surrounding Skull After Brain Implantation
- Surgical Innovation Cuts Ovarian Cancer Risk by 80%
- New Imaging Combo Offers Hope for High-Risk Heart Patients
- New Classification System Brings Clarity to Brain Tumor Surgery Decisions
- Boengineered Tissue Offers New Hope for Secondary Lymphedema Treatment
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- New AI Approach to Improve Surgical Imaging
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- Ultrasound Device Offers Non-Invasive Treatment for Kidney Stones
- Light-Activated Tissue Adhesive Patch Achieves Rapid and Watertight Neurosurgical Sealing
- Minimally Invasive Coronary Artery Bypass Method Offers Safer Alternative to Open-Heart Surgery
- Injectable Breast ‘Implant’ Offers Alternative to Traditional Surgeries
- AI Detects Stomach Cancer Risk from Upper Endoscopic Images
- NIR Light Enables Powering and Communicating with Implantable Medical Devices
- Simple Bypass Protocol Improves Outcomes in Chronic Cerebral Occlusion
Channels
Artificial Intelligence
view channelCritical Care
view channel
AI Stethoscope Spots Heart Valve Disease Earlier Than GPs
Valvular heart disease affects more than half of people over 65, yet it often goes undiagnosed until symptoms become severe. In advanced stages, untreated cases can carry a mortality risk of up to 80%... Read more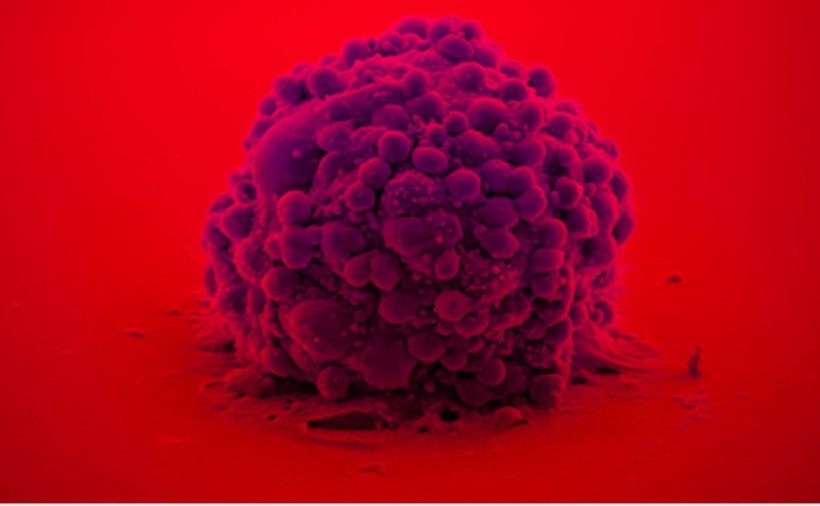
Bioadhesive Patch Eliminates Cancer Cells That Remain After Brain Tumor Surgery
Glioblastoma is the most common and aggressive form of brain tumor, characterized by rapid growth, high invasiveness, and an extremely poor prognosis. Even with surgery followed by radiotherapy and chemotherapy,... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more