Cardiologist Care Reduces Incipient AF Mortality
|
By HospiMedica International staff writers Posted on 12 Dec 2017 |
Specialist care associated is associated with a significantly lower death rate in patients newly diagnosed with atrial fibrillation (AF), according to a new study.
Researchers at the University of Toronto (Canada), the Institute for Clinical Evaluative Sciences (ICES; Toronto, Canada), and other institutions conducted a retrospective study of adult patients with new-onset AF in Ontario (Canada) from 2010 to 2012, in order to assess the association between cardiologist care and clinical outcomes. Patients who saw a cardiologist within one year of initial diagnosis were matched to patients who did not. Main outcomes and measures included death, hospitalization for AF, stroke syndromes, bleeding, and heart failure.
The results revealed that the majority (85%) of new-onset AF patients saw a cardiologist within the year. Cardiologist care within the first year of diagnosis was associated with a lower rate of death (5.3% versus 7.7%) than in those who did not seek care, despite increased hospitalizations for AF (17.9% versus 8.2%), stroke syndromes (1.7% versus 0.5%), bleeding (3.1% versus 2.0%), and heart failure (3.2% versus 1.4%). The results indicate that one in 15 patients with new-onset AF died within a year of the diagnosis. The study was published in the December 2017 issue of the Canadian Journal of Cardiology.
“Variations in AF care across medical specialties are well known. Other than stroke prevention therapy, no other therapy has been associated with improved survival in patients with AF,” said lead author cardiologist Sheldon Singh, MD, of the University of Toronto. “Heart failure and sudden death account for 35-50% of AF deaths, so we hypothesized that comprehensive cardiovascular care beyond stroke prevention may improve overall survival in AF patients.”
“The most startling finding from this study is the high rate of death in the cohort overall. Therefore, a new diagnosis of AF, while not immediately life-threatening, should be regarded as an important marker of near-term risk of cardiovascular events,” commented Stephen Wilton, MD, of the Libin Cardiovascular Institute of Alberta (Calgary, Canada), in an accompanying editorial. “This observation alone provides a potential rationale for desiring early cardiovascular specialist evaluation for these patients.”
AF occurs when the heart's two upper chambers beat erratically. In one form, paroxysmal AF, patients have bouts of erratic beats that begin spontaneously and usually last less than a week. It can lead to serious adverse events such as thrombi traveling from the heart to obstruct arteries supplying the brain, causing stroke, or other parts of the body causing tissue damage.
Related Links:
University of Toronto
Institute for Clinical Evaluative Sciences
Researchers at the University of Toronto (Canada), the Institute for Clinical Evaluative Sciences (ICES; Toronto, Canada), and other institutions conducted a retrospective study of adult patients with new-onset AF in Ontario (Canada) from 2010 to 2012, in order to assess the association between cardiologist care and clinical outcomes. Patients who saw a cardiologist within one year of initial diagnosis were matched to patients who did not. Main outcomes and measures included death, hospitalization for AF, stroke syndromes, bleeding, and heart failure.
The results revealed that the majority (85%) of new-onset AF patients saw a cardiologist within the year. Cardiologist care within the first year of diagnosis was associated with a lower rate of death (5.3% versus 7.7%) than in those who did not seek care, despite increased hospitalizations for AF (17.9% versus 8.2%), stroke syndromes (1.7% versus 0.5%), bleeding (3.1% versus 2.0%), and heart failure (3.2% versus 1.4%). The results indicate that one in 15 patients with new-onset AF died within a year of the diagnosis. The study was published in the December 2017 issue of the Canadian Journal of Cardiology.
“Variations in AF care across medical specialties are well known. Other than stroke prevention therapy, no other therapy has been associated with improved survival in patients with AF,” said lead author cardiologist Sheldon Singh, MD, of the University of Toronto. “Heart failure and sudden death account for 35-50% of AF deaths, so we hypothesized that comprehensive cardiovascular care beyond stroke prevention may improve overall survival in AF patients.”
“The most startling finding from this study is the high rate of death in the cohort overall. Therefore, a new diagnosis of AF, while not immediately life-threatening, should be regarded as an important marker of near-term risk of cardiovascular events,” commented Stephen Wilton, MD, of the Libin Cardiovascular Institute of Alberta (Calgary, Canada), in an accompanying editorial. “This observation alone provides a potential rationale for desiring early cardiovascular specialist evaluation for these patients.”
AF occurs when the heart's two upper chambers beat erratically. In one form, paroxysmal AF, patients have bouts of erratic beats that begin spontaneously and usually last less than a week. It can lead to serious adverse events such as thrombi traveling from the heart to obstruct arteries supplying the brain, causing stroke, or other parts of the body causing tissue damage.
Related Links:
University of Toronto
Institute for Clinical Evaluative Sciences
Latest Critical Care News
- Single Heart Attack Shot to Revolutionize Cardiac Care
- Single Mid-Wave Infrared Thermal Camera Enables Noncontact Vital Signs Monitoring
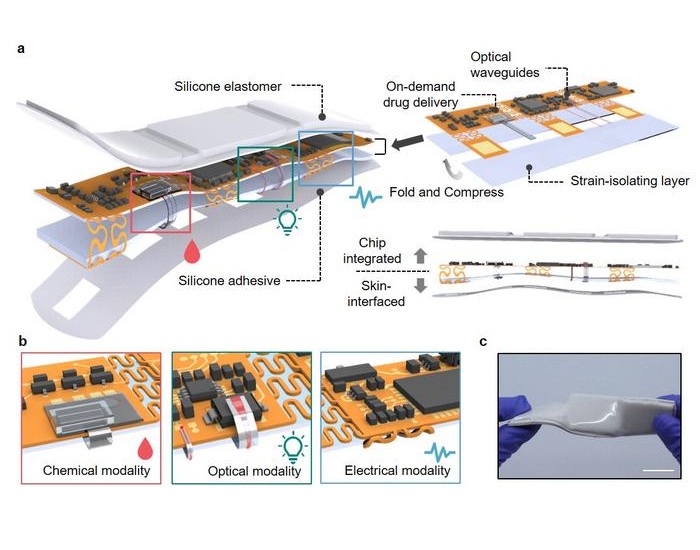
- 3D-Printed Bandage to Help Heal Chronic Wounds
- Ultrasound-Activated Nanoagents Kill Superbugs Hiding in Biofilms
- Painless Microneedle Skin Patch Monitors Immune Health

- Smart T-Shirt Uses AI to Enhance Detection of Heart Rhythm Disorders
- Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
- Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
- AI Model Could Help Diagnose Spinal Cord Disease Up To 30 Months Earlier
- 3D-Printed Swallowable Robot Could Perform Gastrointestinal Procedures
- Next-Gen Hydrogel Could Transform Soft Tissue and Organ Repair
- Engineered Cancer Eating Bacteria Consume Tumors from Inside Out
- ‘Cyborg’ Transplants Could Replace Pancreatic Tissue Damaged by Diabetes
- Smartphone-Linked Catheter Sensor Spots UTIs Sooner Than Lab Cultures
- AI Tool Identifies Trauma Patients Requiring Blood Transfusions Before Reaching Hospital
- New Clinical Guidelines to Reduce Central Line-Associated Bloodstream Infection
Channels
Artificial Intelligence
view channelSurgical Techniques
view channel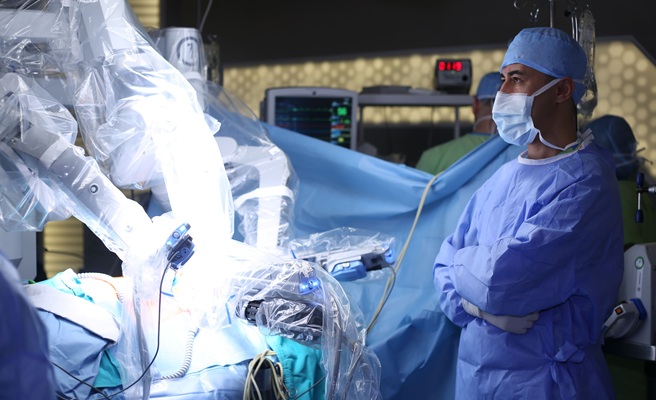
Surgical Robot Makes Complex Liver Tumor Surgery Safer and Less Invasive
Tumors located in the caudate lobe of the liver present a major surgical challenge. This deep section of the liver sits close to critical blood vessels, making traditional surgical access difficult and... Read more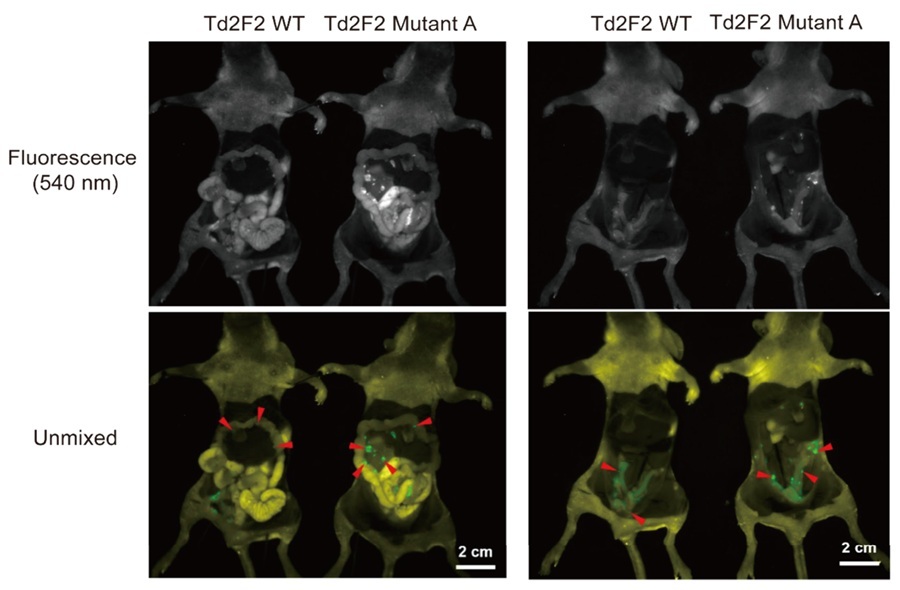
Fluorescence Probe Paired with Engineered Enzymes Lights Up Tumors for Easier Surgical Removal
Successful cancer surgery relies on a surgeon’s ability to remove tumors while preserving as much healthy tissue as possible. To assist with this, surgeons often use fluorescent dyes that cause cancer... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more