DVT Thrombolysis Does Not Prevent Long-Term Complications
|
By HospiMedica International staff writers Posted on 19 Dec 2017 |
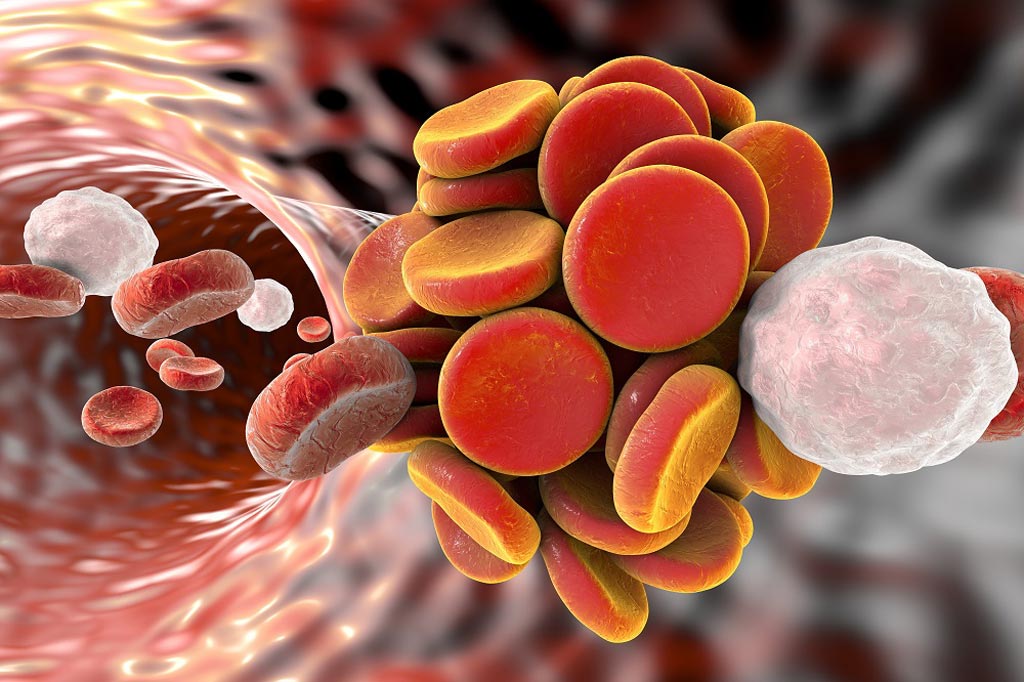
Image: A new study showed moderate-to-severe post-thrombotic syndrome occurred in 18% and 24% of patients in the pharmacomechanical thrombolysis and control groups, respectively (Photo courtesy of SPL).
A new study suggests that pharmacomechanical catheter-directed thrombolysis does not lower the risk of post-thrombotic syndrome in patients with acute proximal deep-vein thrombosis (DVT).
Researchers at McMaster University (Hamilton, ON, Canada), Washington University School of Medicine (WUSTL; St. Louis, MO, USA), and other institutions conducted a study that randomly assigned 692 acute proximal DVT patients to either anticoagulation alone or anticoagulation plus pharmacomechanical thrombolysis, delivered via catheter-mediated or device-mediated intrathrombus delivery of recombinant tissue plasminogen activator (tPA), combined with thrombus aspiration or maceration. The primary outcome was development of post-thrombotic syndrome.
The results revealed that after six to 24 months of follow-up, there was no significant between-group difference in the percentage of patients with the post-thrombotic syndrome. Pharmacomechanical thrombolysis led to five times more major bleeding events within 10 days, but no significant difference in recurrent DVT was seen over the 24-month follow-up period. Moderate-to-severe post-thrombotic syndrome occurred in 18% of patients in the pharmacomechanical thrombolysis group, versus 24% of those in the control group. Improvement in quality of life from baseline to 24 months did not differ significantly between treatment groups. The study was published on December 7, 2017, in the New England Journal of Medicine (NEJM).
“We are dealing with a very sharp double-edged sword here. None of us was surprised to find that this treatment is riskier than blood-thinning drugs alone. To justify that extra risk, we would have had to show a dramatic improvement in long-term outcomes, and the study didn't show that,” said lead author professor Suresh Vedantham, MD, of WUSTL. “What we know now is that we can spare most patients the need to undergo a risky and costly treatment. The findings are also interesting because there is the suggestion that at least some patients may have benefited.”
About 300K- 600K people a year in the United States alone are diagnosed with DVT, and despite standard treatment with blood thinners, roughly half will develop post-thrombotic syndrome, which results from damaged venous valves that become leaky and allow fluid to pool around the ankles. Symptoms include chronic leg pain, swelling, redness, and eventually ulcers. There is no treatment to prevent the potentially debilitating complication.
Related Links:
McMaster University
Washington University School of Medicine
Researchers at McMaster University (Hamilton, ON, Canada), Washington University School of Medicine (WUSTL; St. Louis, MO, USA), and other institutions conducted a study that randomly assigned 692 acute proximal DVT patients to either anticoagulation alone or anticoagulation plus pharmacomechanical thrombolysis, delivered via catheter-mediated or device-mediated intrathrombus delivery of recombinant tissue plasminogen activator (tPA), combined with thrombus aspiration or maceration. The primary outcome was development of post-thrombotic syndrome.
The results revealed that after six to 24 months of follow-up, there was no significant between-group difference in the percentage of patients with the post-thrombotic syndrome. Pharmacomechanical thrombolysis led to five times more major bleeding events within 10 days, but no significant difference in recurrent DVT was seen over the 24-month follow-up period. Moderate-to-severe post-thrombotic syndrome occurred in 18% of patients in the pharmacomechanical thrombolysis group, versus 24% of those in the control group. Improvement in quality of life from baseline to 24 months did not differ significantly between treatment groups. The study was published on December 7, 2017, in the New England Journal of Medicine (NEJM).
“We are dealing with a very sharp double-edged sword here. None of us was surprised to find that this treatment is riskier than blood-thinning drugs alone. To justify that extra risk, we would have had to show a dramatic improvement in long-term outcomes, and the study didn't show that,” said lead author professor Suresh Vedantham, MD, of WUSTL. “What we know now is that we can spare most patients the need to undergo a risky and costly treatment. The findings are also interesting because there is the suggestion that at least some patients may have benefited.”
About 300K- 600K people a year in the United States alone are diagnosed with DVT, and despite standard treatment with blood thinners, roughly half will develop post-thrombotic syndrome, which results from damaged venous valves that become leaky and allow fluid to pool around the ankles. Symptoms include chronic leg pain, swelling, redness, and eventually ulcers. There is no treatment to prevent the potentially debilitating complication.
Related Links:
McMaster University
Washington University School of Medicine
Latest Surgical Techniques News
- 3D Printable Bio-Active Glass Could Serve as Bone Replacement Material
- Spider-Inspired Magnetic Soft Robots to Perform Minimally Invasive GI Tract Procedures
- Micro Imaging Device Paired with Endoscope Spots Cancers at Earlier Stage
- AI Spine Model Could Reduce Surgical Risks
- Novel Method Uses Interstitial Fluid Flow to Predict Where Brain Tumor Can Grow Next
- World’s First Custom Anterior Cervical Spine Surgery Performed Using Personalized Implant
- Implantable Biodegradable Scaffold Helps Broken Bones Regrow Quickly
- First Human Spinal Cord Repair Using Patient Own Cells Could Cure Paralysis
- 'Dual-Mode' Tracer Enables Surgeons to See and Hear Prostate Cancer
- Pioneering One-Stage Hybrid Surgery Ensures Safer Outcomes in Brain and Spine Tumors
- Reimplanting Lab-Grown Patient Cartilage Accelerates Healing After Hip Surgery
- Diamond-Based Sensor Pinpoints Metastasized Cancer for Surgical Removal
- Minimally Invasive Valve Repair Improves Survival in Elderly AFMR Patients
- Tiny Soft Robots Dissolve Painful Kidney Stones with Targeted Drug Delivery
- Implantable 3D Patch Closes and Repairs Heart Defects
- New Endoscopy Technology Enables Early Detection of Esophageal Cancer
Channels
Critical Care
view channel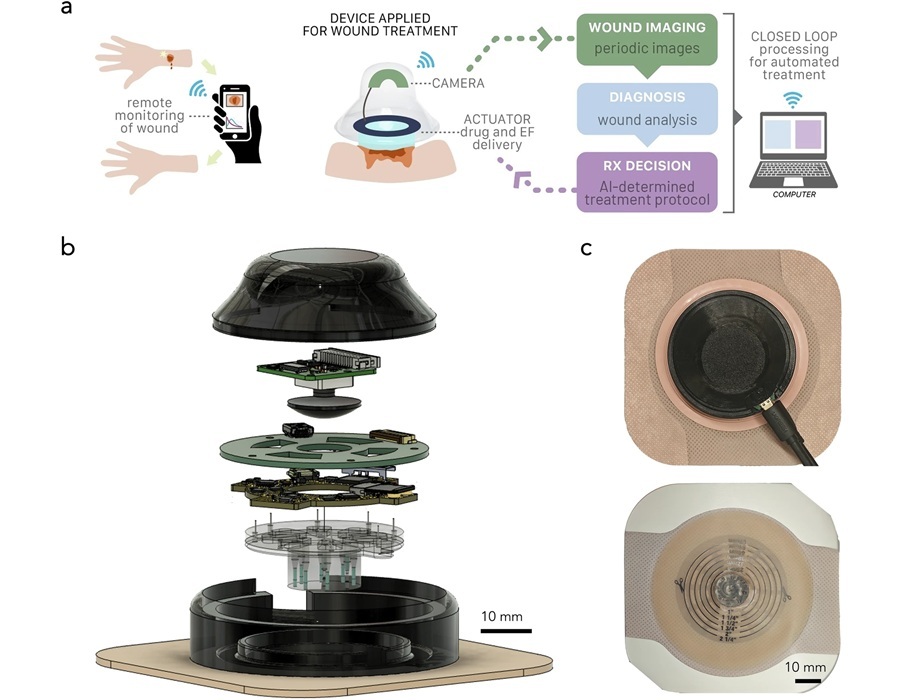
Wearable ‘Microscope in a Bandage’ Fastens Wound Healing
Wound healing is a complex biological process that moves through stages, including clotting, immune response, scabbing, and scarring. For many patients, especially those in remote areas or with limited... Read more
Virus Cocktail to Combat Superbugs Offers New Precision Medicine Approach for Hospitals Battling AMR
Antimicrobial resistance is one of the most pressing challenges in modern medicine, making once-treatable infections increasingly lethal. Enterobacter infections, for example, are difficult to treat and... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
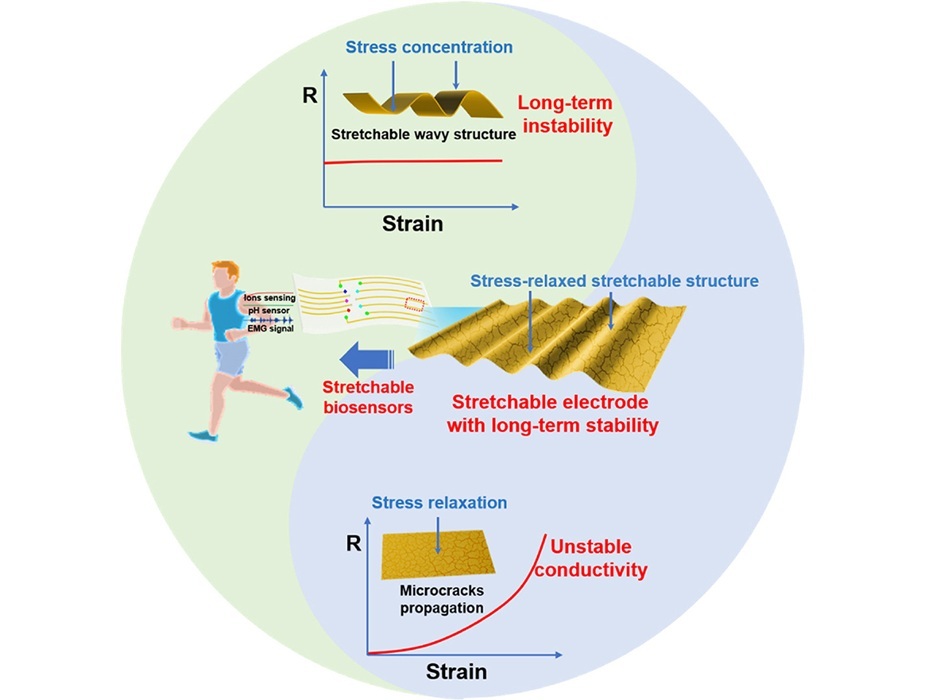
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more