Interactive VR Assists in Treatment Planning
|
By HospiMedica International staff writers Posted on 16 Apr 2018 |
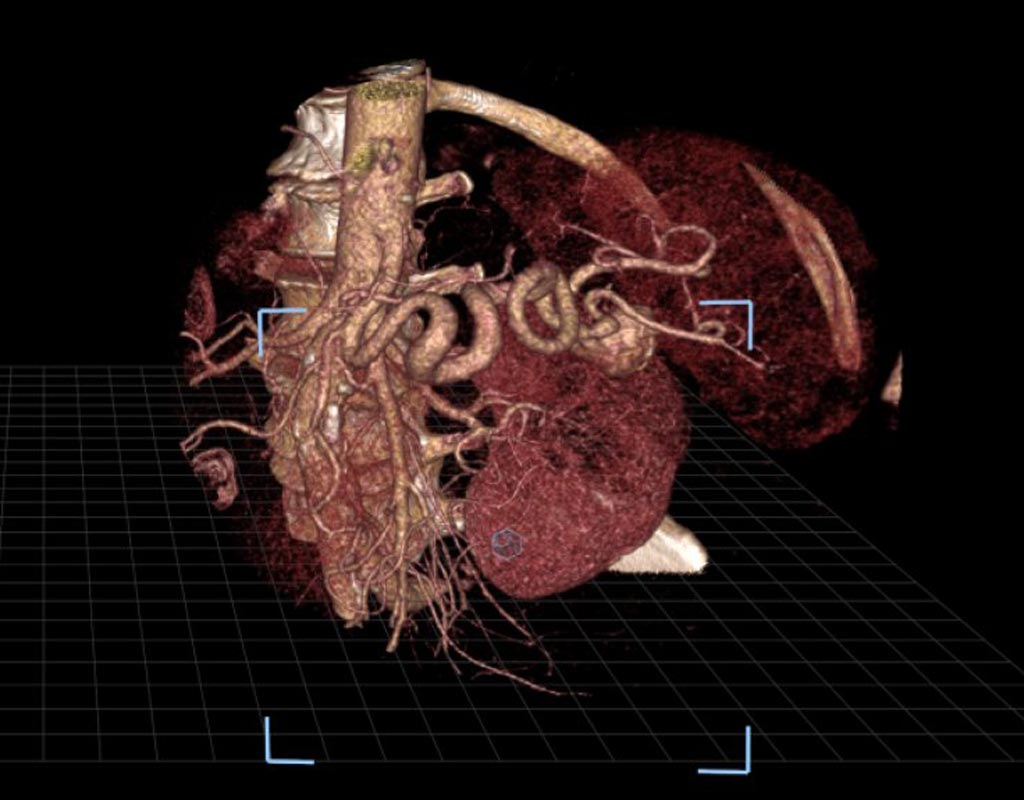
Image: An image of a splenic artery aneurysm as seen in virtual reality (Photo courtesy of SIR).
Interactive virtual reality (VR) shows a patient's unique internal anatomy to interventional radiologists in order to help physicians effectively prepare and tailor their approach to complex treatments, such as splenic artery aneurysm repair. In a new study, researchers compared the VR technology to the use of images from a commonly used visualization software system that displays images on a standard two-dimensional platform and found the accuracy to be similar with both methods, though confidence improved substantially with VR.
VR converts a patient's pre-procedural CT scans into 3D images that can be virtually moved and examined by radiologists wearing virtual reality-type glasses. VR allows operators to manipulate routine, two-dimensional images in an open three-dimensional space in order to allow them to look into the patients' organs and tissues that had been impossible outside of the human body, until now. This arms the operators with a deeper and intuitive understanding of spatial relationships, such as between an aneurysm and the surrounding arteries.
In the study, three radiologists used both the technologies to independently evaluate 17 splenic artery aneurysms in 14 patients. The researchers measured the accuracy of the radiologists in identifying inflow and outflow arteries associated with the aneurysms with each method. The radiologists also ranked improvements in their confidence on a four-point scale when using VR as compared to the standard method. The researchers found that 93% of the participating physicians who used the VR method indicated higher confidence in their abilities (a score of at least three).
"Treating splenic artery aneurysms can be very difficult because of their intricate nature and anatomic variations from patient to patient. This new platform allows you to view a patient's arterial anatomy in a three-dimensional image, as if it is right in front of you, which may help interventional radiologists more quickly and thoroughly plan for the equipment and tools they'll need for a successful outcome," said Zlatko Devcic, M.D., a fellow of interventional radiology at Stanford University School of Medicine and collaborating author of the study. "Pre-operative planning is possibly the most important step towards successfully treating a patient, so the value of VR cannot be understated," Devcic said. "This technology gives us a totally different way to look at that structure and safely plan our approach to patient care."
The research was presented at the Society of Interventional Radiology's 2018 Annual Scientific Meeting. The researchers hope that more studies in the future will examine whether the VR technology will ultimately help reduce the time required to perform the treatment and consequently, reduce the amount of radiation and contrast exposure to the patient.
VR converts a patient's pre-procedural CT scans into 3D images that can be virtually moved and examined by radiologists wearing virtual reality-type glasses. VR allows operators to manipulate routine, two-dimensional images in an open three-dimensional space in order to allow them to look into the patients' organs and tissues that had been impossible outside of the human body, until now. This arms the operators with a deeper and intuitive understanding of spatial relationships, such as between an aneurysm and the surrounding arteries.
In the study, three radiologists used both the technologies to independently evaluate 17 splenic artery aneurysms in 14 patients. The researchers measured the accuracy of the radiologists in identifying inflow and outflow arteries associated with the aneurysms with each method. The radiologists also ranked improvements in their confidence on a four-point scale when using VR as compared to the standard method. The researchers found that 93% of the participating physicians who used the VR method indicated higher confidence in their abilities (a score of at least three).
"Treating splenic artery aneurysms can be very difficult because of their intricate nature and anatomic variations from patient to patient. This new platform allows you to view a patient's arterial anatomy in a three-dimensional image, as if it is right in front of you, which may help interventional radiologists more quickly and thoroughly plan for the equipment and tools they'll need for a successful outcome," said Zlatko Devcic, M.D., a fellow of interventional radiology at Stanford University School of Medicine and collaborating author of the study. "Pre-operative planning is possibly the most important step towards successfully treating a patient, so the value of VR cannot be understated," Devcic said. "This technology gives us a totally different way to look at that structure and safely plan our approach to patient care."
The research was presented at the Society of Interventional Radiology's 2018 Annual Scientific Meeting. The researchers hope that more studies in the future will examine whether the VR technology will ultimately help reduce the time required to perform the treatment and consequently, reduce the amount of radiation and contrast exposure to the patient.
Latest Business News
- Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
- B. Braun Acquires Digital Microsurgery Company True Digital Surgery
- CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
- Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
- Medtronic Partners with Corsano to Expand Acute Care & Monitoring Portfolio in Europe
- Expanded Collaboration to Transform OR Technology Through AI and Automation
- Becton Dickinson to Spin Out Biosciences and Diagnostic Solutions Business
- Boston Scientific Acquires Medical Device Company SoniVie
- 2026 World Hospital Congress to be Held in Seoul
- Teleflex to Acquire BIOTRONIK’s Vascular Intervention Business
- Philips and Mass General Brigham Collaborate on Improving Patient Care with Live AI-Powered Insights
- Arab Health 2025 Celebrates Landmark 50th Edition
- Boston Scientific Acquires Medical Device Company Intera Oncology
- MEDICA 2024 to Highlight Hot Topics of MedTech Industry
- Start-Ups To Once Again Play Starring Role at MEDICA 2024
- Boston Scientific to Acquire AFib Ablation Company Cortex
Channels
Critical Care
view channel
Swallowable Pill-Sized Bioprinter Treats GI Tract Injuries
Soft tissue injuries in the gastrointestinal tract, such as ulcers and hemorrhages, are typically treated through invasive surgical procedures that carry high risks and do not always result in permanent repair.... Read more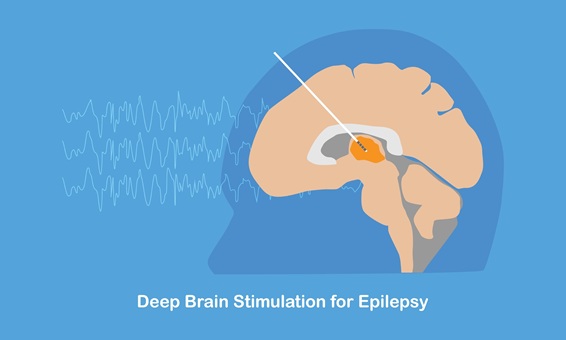
Personalized Brain “Pacemakers” Could Help Patients with Hard-To-Treat Epilepsy
Epilepsy affects more than 50 million people worldwide, and nearly one-third of them do not respond to available medications. For many patients, seizures originate in brain areas responsible for essential... Read moreSurgical Techniques
view channel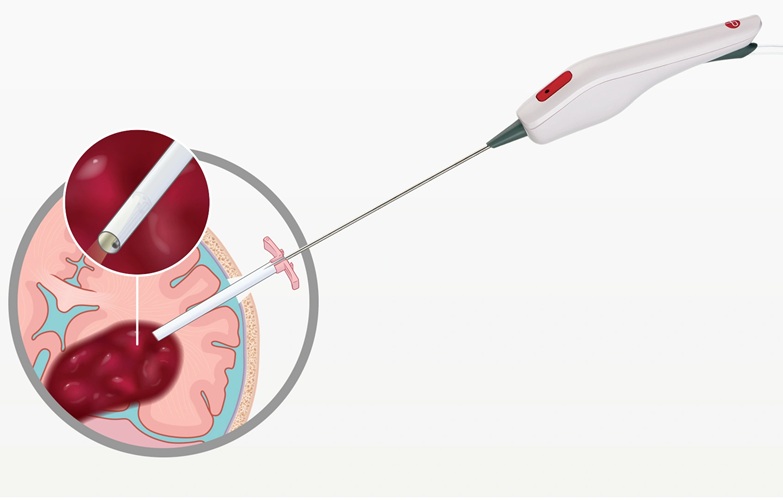
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel