Pre-Op Weight Loss Improves Bariatric Surgery Outcomes
|
By HospiMedica International staff writers Posted on 25 Apr 2018 |

Image: A new study shows losing weight before bariartic surgery improves surgical outcomes (Photo courtesy of 123RF).
Patients who lost at least 8% of their excess weight through a low-calorie diet (LCD) immediately before bariatric surgery have more successful long-term outcomes, according to a new study.
Researchers at the Greenville Health System (GHS; Greenville, SC, USA) conducted a study to determine the effect of preoperative excess weight loss (EWL) on postoperative outcomes in 355 patients undergoing primary vertical sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) between 2014 and 2016. The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. All patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
The LCD was observed for four weeks immediately preceding surgery. The patients were then divided into two cohorts and analyzed according to those who achieved an 8% or higher EWL (224 patients), and those who did not (131 patients). The primary endpoints included percent excess weight loss (% EWL) at 1, 3, 6, and 12 months postoperatively. The results revealed that patients who achieved an 8% or higher EWL were more successful at continued weight loss during the first year after surgery than the patients who did not lose as much weight preoperatively.
The cohort that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively), a higher proportion of white patients (84.8% vs. 74.1%), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%). The two groups had similar rates of preoperative comorbidities and surgery types. In addition, those who achieved the target weight loss had a shorter hospital stay and a higher % EWL at three months, six months, and one year post-operatively. The study was published in the April 2018 issue of the Journal of the American College of Surgeons (JACS).
“These findings suggest that surgeons and clinical care teams should encourage healthy eating and exercise. The program helped patients establish healthy eating habits, establish portion control and learn what a healthy meal looks like,” said lead author clinical nutrition specialist Deborah Hutcheon, DCN. “Weight loss from the liver and abdominal cavity helps to improve surgical access, which may be why surgical times and recovery periods went down.”
“We call it the honeymoon period of bariatric surgery. After a year or year and a half, your body starts to figure out what it can and can’t do, and your behaviors may change a little bit, so the odds that you are going to lose a significant amount of weight after that time period are definitely decreased,” said senior author John Scott, MD. “Therefore, the more weight you can lose during that honeymoon period, the better, because that effort will help establish a set point, in terms of where your steady weight is going to be further down the road.”
Related Links:
Greenville Health System
Researchers at the Greenville Health System (GHS; Greenville, SC, USA) conducted a study to determine the effect of preoperative excess weight loss (EWL) on postoperative outcomes in 355 patients undergoing primary vertical sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) between 2014 and 2016. The LCD included 1,200 kcal/day (45% carbohydrates, 35% protein, 20% fat), which were consumed through five meal-replacement products and one food-based meal. All patients were also instructed to conduct 30 minutes of moderate to vigorous activity per day.
The LCD was observed for four weeks immediately preceding surgery. The patients were then divided into two cohorts and analyzed according to those who achieved an 8% or higher EWL (224 patients), and those who did not (131 patients). The primary endpoints included percent excess weight loss (% EWL) at 1, 3, 6, and 12 months postoperatively. The results revealed that patients who achieved an 8% or higher EWL were more successful at continued weight loss during the first year after surgery than the patients who did not lose as much weight preoperatively.
The cohort that achieved the target contained a greater proportion of men than did the other group (25.5% vs. 13.7%, respectively), a higher proportion of white patients (84.8% vs. 74.1%), and a higher proportion of patients taking antihypertensive medications (68.3% vs. 57.3%). The two groups had similar rates of preoperative comorbidities and surgery types. In addition, those who achieved the target weight loss had a shorter hospital stay and a higher % EWL at three months, six months, and one year post-operatively. The study was published in the April 2018 issue of the Journal of the American College of Surgeons (JACS).
“These findings suggest that surgeons and clinical care teams should encourage healthy eating and exercise. The program helped patients establish healthy eating habits, establish portion control and learn what a healthy meal looks like,” said lead author clinical nutrition specialist Deborah Hutcheon, DCN. “Weight loss from the liver and abdominal cavity helps to improve surgical access, which may be why surgical times and recovery periods went down.”
“We call it the honeymoon period of bariatric surgery. After a year or year and a half, your body starts to figure out what it can and can’t do, and your behaviors may change a little bit, so the odds that you are going to lose a significant amount of weight after that time period are definitely decreased,” said senior author John Scott, MD. “Therefore, the more weight you can lose during that honeymoon period, the better, because that effort will help establish a set point, in terms of where your steady weight is going to be further down the road.”
Related Links:
Greenville Health System
Latest Surgical Techniques News
- Minimally Invasive Coronary Artery Bypass Method Offers Safer Alternative to Open-Heart Surgery
- Injectable Breast ‘Implant’ Offers Alternative to Traditional Surgeries
- AI Detects Stomach Cancer Risk from Upper Endoscopic Images
- NIR Light Enables Powering and Communicating with Implantable Medical Devices
- Simple Bypass Protocol Improves Outcomes in Chronic Cerebral Occlusion
- Implantable Absorbable Sensor Detects Life-Threatening Complications After Intestinal Surgery
- New Study Findings Enable Improved Ventilation During Complex Lung Surgery
- 3D-Printed Blood Vessel Scaffolds Could Transform Heart Bypass Surgeries
- Novel Imaging Technique Helps View Blood Perfusion During Esophageal Surgery
- Minimally Invasive Surgery Proven Safe and Effective for Complex ‘Whipple’ Procedure
- Catheter-Based Procedures Offer Less Invasive Option for Treatment of Valvular Disease
- Laparoscopic Surgery Improves Outcomes for Severe Newborn Liver Disease
- Novel Endoscopy Technique Provides Access to Deep Lung Tumors
- New Study Findings Could Halve Number of Stent Procedures
- Breakthrough Surgical Device Redefines Hip Arthroscopy
- Automated System Enables Real-Time "Molecular Pathology" During Cancer Surgery
Channels
Critical Care
view channel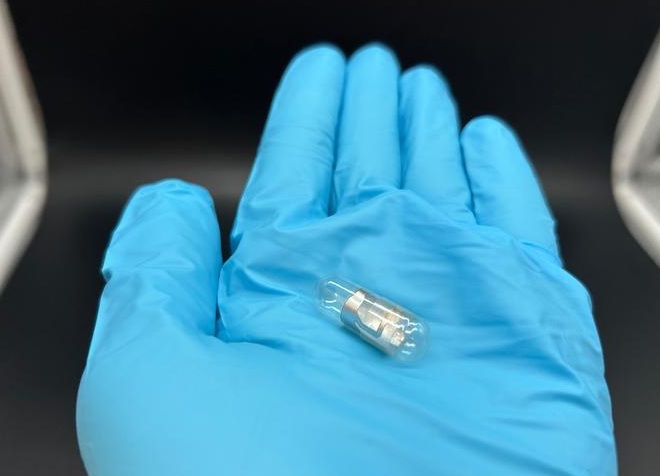
Pill Reports from Stomach When It Has Been Swallowed
Failure to take medications on time is a major challenge in healthcare and contributes to hundreds of thousands of preventable deaths and billions of dollars in avoidable costs each year.... Read more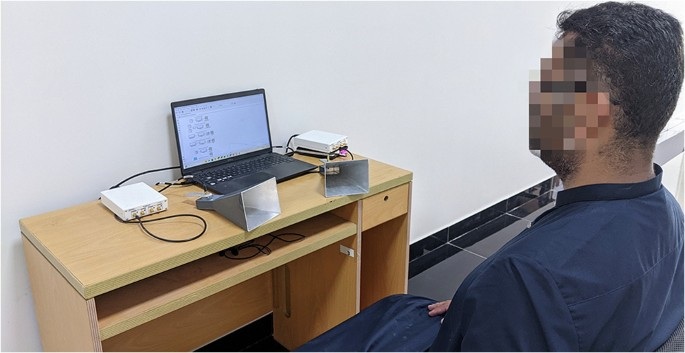
Wireless Sensing Technology Enables Touch-Free Diagnostics of Common Lung Diseases
Diagnosing lung diseases often requires physical contact, imaging scans, or specialized equipment, which can limit access in low-resource settings and increase infection risk during outbreaks.... Read more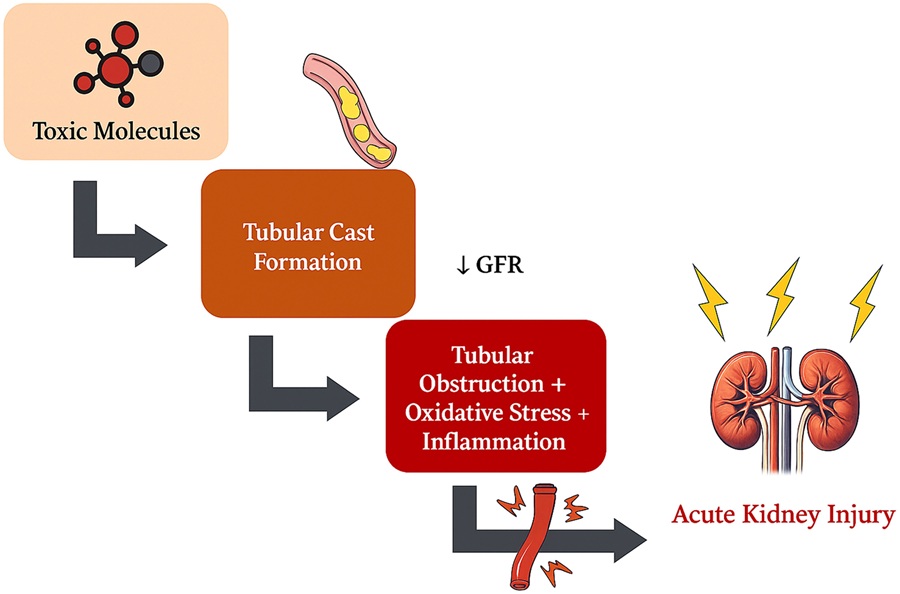
Early Detection and Targeted Blood Purification Could Prevent Kidney Failure in ICU Patients
Acute kidney injury (AKI) is one of the most dangerous complications in intensive care units, affecting up to half of critically ill patients and sharply increasing mortality risk. A common but preventable... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
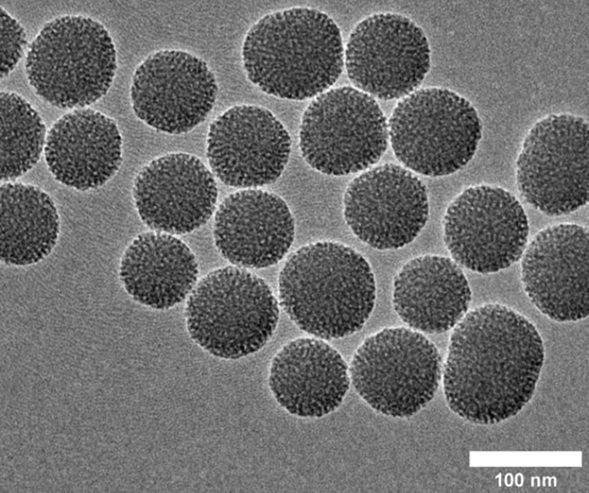
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more