Cross-Checking between ED Physicians Reduces Harm
|
By HospiMedica International staff writers Posted on 08 May 2018 |

Image: A new study suggests a few minutes of consultation can avoid adverse ED events (Photo courtesy of Dreamstime).
A new study suggests that systematic cross-checking between doctors may be a key to reducing the high rate of adverse events in the emergency department (ED).
Researchers at the Sorbonne University (Paris, France), Pitie-Salpetriere Hospital (Paris, France), and other institutions conducted a cluster randomized crossover trial that included a random sample of 1,680 patients attended to in six EDs in France during two 10-day periods. The intervention included systematic cross-checking between ED physicians three times a day, which included a brief presentation of one physician’s case to another, followed by the second physician’s feedback. The main outcome was medical error, defined as either a near miss or a serious adverse event.
The results showed that there were 54 adverse events among 840 patients (6.4%) during the cross-check intervention, compared with 90 adverse events among 840 patients (10.7%) during the control period, a relative reduction of 40%. Most of the reductions occurred in adverse events defined as near misses, with a reduction of 47%. Errors in sepsis management accounted for more than 40% of the preventable serious adverse events. The median duration of cross-checking sessions was nine minutes, during which about seven patients were discussed. The study was published on April 23, 2018, in JAMA Internal Medicine.
“The reduction in preventable serious adverse events with systematic cross-checking did not reach statistical significance; only reductions in near misses did,” explained lead author Yonathan Freund, MD, PhD, of Hôpital Pitié-Salpêtrière. “Whether an adverse event resulted from a misdiagnosis or from the implementation of an inappropriate plan for the correct diagnosis could not be determined decisively. This included sepsis-associated medical errors, which may be particularly relevant, because the most commonly occurring serious adverse events were violations of the surviving sepsis campaign guidelines.”
An adverse event is defined as a preventable or non-preventable injury that was caused by medical management (rather than the underlying disease) and that prolonged hospitalization, produced a disability at the time of discharge, or both. Adverse event also include errors, defined as acts of commission or omission leading to an undesirable outcome or significant potential for such an outcome, and near misses, in which an error was committed, but the patient did not experience clinical harm, either through early detection or sheer luck.
Related Links:
Sorbonne University
Pitie-Salpetriere Hospital
Researchers at the Sorbonne University (Paris, France), Pitie-Salpetriere Hospital (Paris, France), and other institutions conducted a cluster randomized crossover trial that included a random sample of 1,680 patients attended to in six EDs in France during two 10-day periods. The intervention included systematic cross-checking between ED physicians three times a day, which included a brief presentation of one physician’s case to another, followed by the second physician’s feedback. The main outcome was medical error, defined as either a near miss or a serious adverse event.
The results showed that there were 54 adverse events among 840 patients (6.4%) during the cross-check intervention, compared with 90 adverse events among 840 patients (10.7%) during the control period, a relative reduction of 40%. Most of the reductions occurred in adverse events defined as near misses, with a reduction of 47%. Errors in sepsis management accounted for more than 40% of the preventable serious adverse events. The median duration of cross-checking sessions was nine minutes, during which about seven patients were discussed. The study was published on April 23, 2018, in JAMA Internal Medicine.
“The reduction in preventable serious adverse events with systematic cross-checking did not reach statistical significance; only reductions in near misses did,” explained lead author Yonathan Freund, MD, PhD, of Hôpital Pitié-Salpêtrière. “Whether an adverse event resulted from a misdiagnosis or from the implementation of an inappropriate plan for the correct diagnosis could not be determined decisively. This included sepsis-associated medical errors, which may be particularly relevant, because the most commonly occurring serious adverse events were violations of the surviving sepsis campaign guidelines.”
An adverse event is defined as a preventable or non-preventable injury that was caused by medical management (rather than the underlying disease) and that prolonged hospitalization, produced a disability at the time of discharge, or both. Adverse event also include errors, defined as acts of commission or omission leading to an undesirable outcome or significant potential for such an outcome, and near misses, in which an error was committed, but the patient did not experience clinical harm, either through early detection or sheer luck.
Related Links:
Sorbonne University
Pitie-Salpetriere Hospital
Latest Critical Care News
- Painless Microneedle Skin Patch Monitors Immune Health

- Smart T-Shirt Uses AI to Enhance Detection of Heart Rhythm Disorders
- Aptamers Enable Real-Time Biomarker Tracking Without Blood Draws
- Specialized Dressing with Sensor Monitors pH Levels in Chronic Wounds
- AI Model Could Help Diagnose Spinal Cord Disease Up To 30 Months Earlier
- 3D-Printed Swallowable Robot Could Perform Gastrointestinal Procedures
- Next-Gen Hydrogel Could Transform Soft Tissue and Organ Repair
- Engineered Cancer Eating Bacteria Consume Tumors from Inside Out
- ‘Cyborg’ Transplants Could Replace Pancreatic Tissue Damaged by Diabetes
- Smartphone-Linked Catheter Sensor Spots UTIs Sooner Than Lab Cultures
- AI Tool Identifies Trauma Patients Requiring Blood Transfusions Before Reaching Hospital
- New Clinical Guidelines to Reduce Central Line-Associated Bloodstream Infection
- New Inhalable Treatment for TB Lowers Side Effects
- AI Algorithm Improves Antibiotic Decision-Making in Urinary Tract Infection
- 3D-Printed System Enhances Vaccine Delivery Via Microneedle Array Patch
- Whole-Heart Mapping Technology Provides Comprehensive Real-Time View of Arrhythmias
Channels
Artificial Intelligence
view channelSurgical Techniques
view channel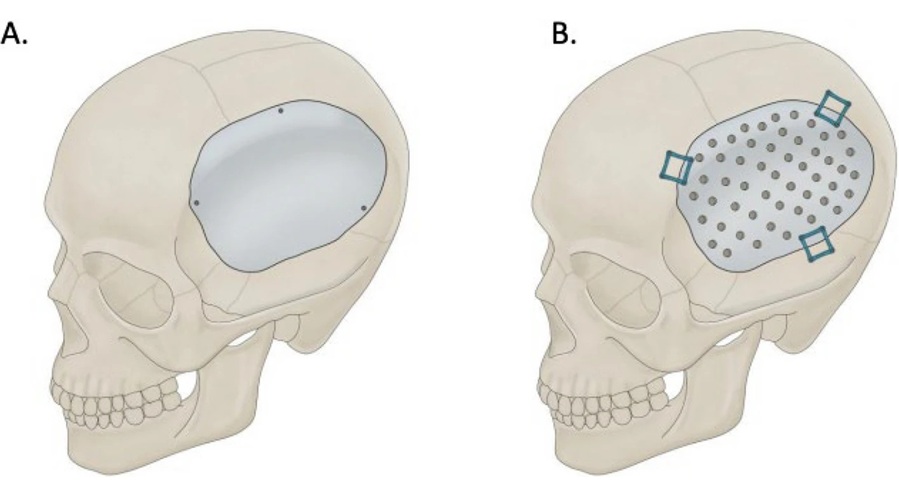
Skull Implant Design Could Shape Surgical Outcomes
Cranioplasty is a common neurosurgical procedure performed to repair skull defects after decompressive craniectomy. In addition to restoring protection to the brain, the surgery can enhance neurological... Read more
Redesigned Surgical Laser Cuts Bone Deeper and Faster Than Before
Lasers are valued in surgery for their precision and non-contact cutting, reducing mechanical stress and minimizing microcracks. While widely used for soft tissue, their application in hard tissues such... Read more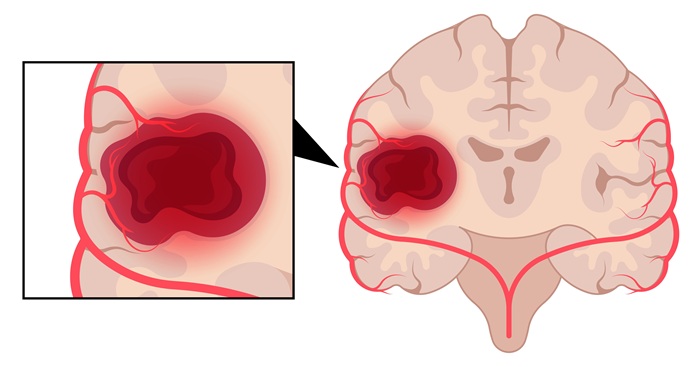
Laser Ablation Plus Immunotherapy Improves Survival in Recurrent Glioblastoma
Recurrent high-grade astrocytoma, including glioblastoma, is difficult to treat and often returns after surgery. Patients with recurrence typically survive only four to five months, highlighting a critical... Read more
New Method Offers Less Invasive Detection of Susceptibility to Rare Anesthesia Reaction
Malignant hyperthermia (MH) is a rare, inherited reaction to general anesthetics that can be rapidly fatal without prompt recognition and treatment. Definitive preoperative testing today relies on an open... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more