HIE Adoption Improves Patient Transfer Outcomes
|
By HospiMedica International staff writers Posted on 31 Jul 2018 |
A new study concludes that implementing health information exchange (HIE) protocols during inter-hospital transfers reduces diagnostic discordance and improves survival rates.
Researchers at the University of Minnesota (UMN; Minneapolis, USA) and Mayo Clinic Florida (Jacksonville, USA) conducted a study involving 180,337 adult patients transferred between 473 acute care hospitals in the states of New York, Vermont, Florida, Indiana, and Utah from 2011 to 2013. Diagnosis coding before and after hospital transfer was merged with data from the American Hospital Association (Washington, DC, USA; www.aha.org) to examine the frequency and impact of changes in diagnosis on patient risk, and whether HIE can improve patient safety by enhancing diagnostic accuracy.
The results revealed that discordance in diagnoses occurred in 85.5% of all patients; 73% of patients gained a new diagnosis following transfer, while 47% of patients lost a diagnosis. But while diagnostic discordance was associated with increased inpatient mortality, it also allowed for improved mortality prediction. The study also revealed that bilateral hospital HIE participation was associated with reduced diagnostic discordance index and decreased inpatient mortality. The study was published on May 29, 2018, in the Journal of General Internal Medicine.
“The more people that are involved in coordinating care, and the greater number of conversations that have to happen, the more potential there is for breakdowns in communication,” said lead author Michael Usher, MD, PhD, of the UMN division of general internal medicine. “The ability of two hospitals to talk to each other has the potential to improve patient safety, make care much more cost effective, and reduce mortality.”
HIE provides the capability to electronically move clinical information among different information systems, facilitating access to and retrieval of clinical data to provide a safer, more timely, efficient, effective, and equitable continuity of care, and reduced diagnostic tests and imaging. Other benefits include reduced expenses associated with manual printing, scanning, and faxing of documents; physical mailing of patient charts and records; and verification of delivery of referrals, records, and test results.
Related Links:
University of Minnesota
Mayo Clinic Florida
Researchers at the University of Minnesota (UMN; Minneapolis, USA) and Mayo Clinic Florida (Jacksonville, USA) conducted a study involving 180,337 adult patients transferred between 473 acute care hospitals in the states of New York, Vermont, Florida, Indiana, and Utah from 2011 to 2013. Diagnosis coding before and after hospital transfer was merged with data from the American Hospital Association (Washington, DC, USA; www.aha.org) to examine the frequency and impact of changes in diagnosis on patient risk, and whether HIE can improve patient safety by enhancing diagnostic accuracy.
The results revealed that discordance in diagnoses occurred in 85.5% of all patients; 73% of patients gained a new diagnosis following transfer, while 47% of patients lost a diagnosis. But while diagnostic discordance was associated with increased inpatient mortality, it also allowed for improved mortality prediction. The study also revealed that bilateral hospital HIE participation was associated with reduced diagnostic discordance index and decreased inpatient mortality. The study was published on May 29, 2018, in the Journal of General Internal Medicine.
“The more people that are involved in coordinating care, and the greater number of conversations that have to happen, the more potential there is for breakdowns in communication,” said lead author Michael Usher, MD, PhD, of the UMN division of general internal medicine. “The ability of two hospitals to talk to each other has the potential to improve patient safety, make care much more cost effective, and reduce mortality.”
HIE provides the capability to electronically move clinical information among different information systems, facilitating access to and retrieval of clinical data to provide a safer, more timely, efficient, effective, and equitable continuity of care, and reduced diagnostic tests and imaging. Other benefits include reduced expenses associated with manual printing, scanning, and faxing of documents; physical mailing of patient charts and records; and verification of delivery of referrals, records, and test results.
Related Links:
University of Minnesota
Mayo Clinic Florida
Latest Health IT News
Channels
Critical Care
view channel
AI Improves Prediction of CKD Progression to End Stage Renal Disease
Chronic kidney disease (CKD) is a progressive condition that can lead to end-stage renal disease (ESRD), when kidney function drops to critically low levels. Globally, CKD affects between 8% and 16% of... Read more
First-Of-Its-Kind Online Tool to Revolutionize Treatment of High Blood Pressure
High blood pressure affects as many as 1.3 billion people and leads to around ten million deaths each year. Often called a silent killer, it can remain hidden until it causes heart attack, stroke, or kidney... Read moreSurgical Techniques
view channel
World’s First Custom Anterior Cervical Spine Surgery Performed Using Personalized Implant
Anterior cervical fusion has been performed since the 1950s and is one of the most common spine procedures. Traditional implants are designed as one-size-fits-all, which can affect spinal alignment, healing,... Read more
Implantable Biodegradable Scaffold Helps Broken Bones Regrow Quickly
For most broken bones, natural healing occurs while the patient wears a cast or brace. However, severe or complex fractures often require surgical intervention with grafts, scaffolds, or metal fixation... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreBusiness
view channel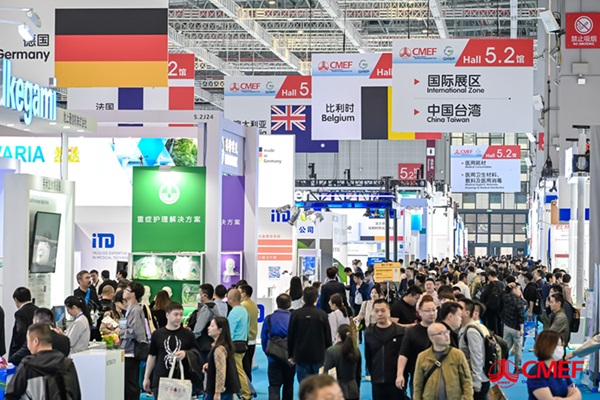
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more
Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
A research collaboration will focus on the joint discovery of novel therapeutic approaches based on findings in human genomics research related to cardiovascular diseases. Bayer (Berlin, Germany) and... Read more