HIE Adoption Improves Patient Transfer Outcomes
|
By HospiMedica International staff writers Posted on 31 Jul 2018 |
A new study concludes that implementing health information exchange (HIE) protocols during inter-hospital transfers reduces diagnostic discordance and improves survival rates.
Researchers at the University of Minnesota (UMN; Minneapolis, USA) and Mayo Clinic Florida (Jacksonville, USA) conducted a study involving 180,337 adult patients transferred between 473 acute care hospitals in the states of New York, Vermont, Florida, Indiana, and Utah from 2011 to 2013. Diagnosis coding before and after hospital transfer was merged with data from the American Hospital Association (Washington, DC, USA; www.aha.org) to examine the frequency and impact of changes in diagnosis on patient risk, and whether HIE can improve patient safety by enhancing diagnostic accuracy.
The results revealed that discordance in diagnoses occurred in 85.5% of all patients; 73% of patients gained a new diagnosis following transfer, while 47% of patients lost a diagnosis. But while diagnostic discordance was associated with increased inpatient mortality, it also allowed for improved mortality prediction. The study also revealed that bilateral hospital HIE participation was associated with reduced diagnostic discordance index and decreased inpatient mortality. The study was published on May 29, 2018, in the Journal of General Internal Medicine.
“The more people that are involved in coordinating care, and the greater number of conversations that have to happen, the more potential there is for breakdowns in communication,” said lead author Michael Usher, MD, PhD, of the UMN division of general internal medicine. “The ability of two hospitals to talk to each other has the potential to improve patient safety, make care much more cost effective, and reduce mortality.”
HIE provides the capability to electronically move clinical information among different information systems, facilitating access to and retrieval of clinical data to provide a safer, more timely, efficient, effective, and equitable continuity of care, and reduced diagnostic tests and imaging. Other benefits include reduced expenses associated with manual printing, scanning, and faxing of documents; physical mailing of patient charts and records; and verification of delivery of referrals, records, and test results.
Related Links:
University of Minnesota
Mayo Clinic Florida
Researchers at the University of Minnesota (UMN; Minneapolis, USA) and Mayo Clinic Florida (Jacksonville, USA) conducted a study involving 180,337 adult patients transferred between 473 acute care hospitals in the states of New York, Vermont, Florida, Indiana, and Utah from 2011 to 2013. Diagnosis coding before and after hospital transfer was merged with data from the American Hospital Association (Washington, DC, USA; www.aha.org) to examine the frequency and impact of changes in diagnosis on patient risk, and whether HIE can improve patient safety by enhancing diagnostic accuracy.
The results revealed that discordance in diagnoses occurred in 85.5% of all patients; 73% of patients gained a new diagnosis following transfer, while 47% of patients lost a diagnosis. But while diagnostic discordance was associated with increased inpatient mortality, it also allowed for improved mortality prediction. The study also revealed that bilateral hospital HIE participation was associated with reduced diagnostic discordance index and decreased inpatient mortality. The study was published on May 29, 2018, in the Journal of General Internal Medicine.
“The more people that are involved in coordinating care, and the greater number of conversations that have to happen, the more potential there is for breakdowns in communication,” said lead author Michael Usher, MD, PhD, of the UMN division of general internal medicine. “The ability of two hospitals to talk to each other has the potential to improve patient safety, make care much more cost effective, and reduce mortality.”
HIE provides the capability to electronically move clinical information among different information systems, facilitating access to and retrieval of clinical data to provide a safer, more timely, efficient, effective, and equitable continuity of care, and reduced diagnostic tests and imaging. Other benefits include reduced expenses associated with manual printing, scanning, and faxing of documents; physical mailing of patient charts and records; and verification of delivery of referrals, records, and test results.
Related Links:
University of Minnesota
Mayo Clinic Florida
Channels
Critical Care
view channel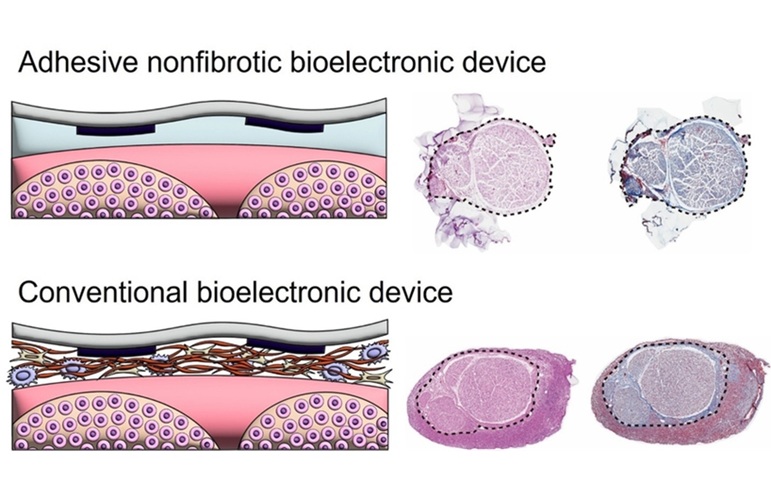
Bioadhesive Strategy Prevents Fibrosis Around Device Implants on Peripheral Nerves
Peripheral nerves connect the brain and spinal cord to muscles, organs, and sensory systems, making them key targets for treating neurological and systemic diseases. However, implantable bioelectronic... Read more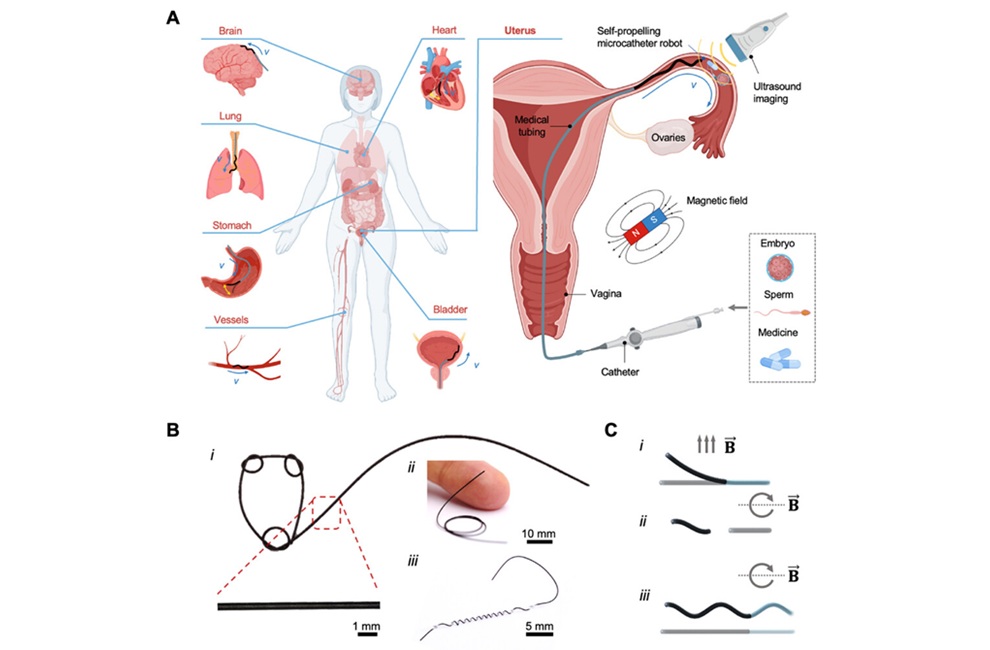
Miniature Non-Invasive Robotic Catheters to Improve Infertility Treatments
Minimally invasive procedures in reproductive and gynaecological medicine are often limited by the difficulty of navigating narrow, delicate anatomical pathways without damaging surrounding tissue.... Read moreSurgical Techniques
view channel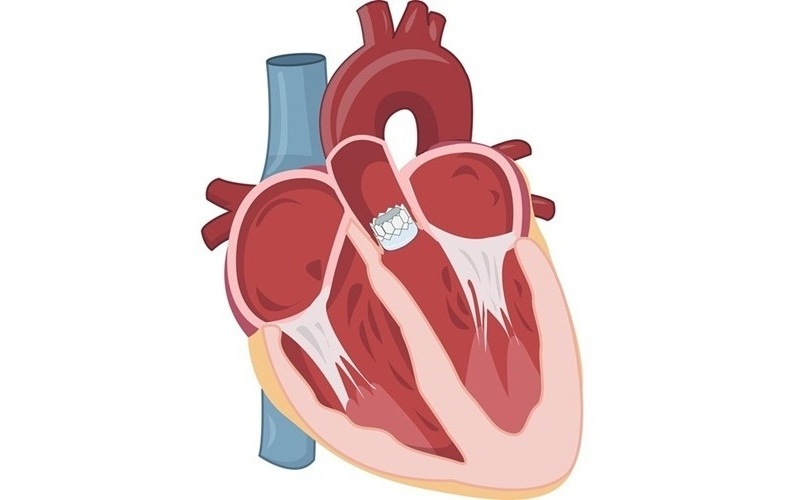
Catheter-Based Procedures Offer Less Invasive Option for Treatment of Valvular Disease
Valvular heart disease, caused by tight or leaky valves between heart chambers, affects up to 10% of older adults and leads to more than 120,000 deaths globally each year. Traditional open-heart surgery... Read moreLaparoscopic Surgery Improves Outcomes for Severe Newborn Liver Disease
Biliary atresia is a rare but life-threatening liver condition in newborns that blocks bile flow and leads to progressive liver damage if not treated early. Surgery is typically performed within the first... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more














