Removing More Blood Improves Hemorrhagic Stroke Recovery
|
By HospiMedica International staff writers Posted on 26 Feb 2019 |

Image: Professor Issam Awad demonstrating the MISTIE procedure (Photo courtesy of University of Chicago).
The greater the volume of blood removed from the brain following cerebral hemorrhage, the greater the odds of better functional recovery, claims a new study.
Researchers at Johns Hopkins University (JHU; Baltimore, MD, USA), the University of Chicago (IL, USA), and 76 other hospitals in the USA, Canada, Europe, Australia, and Asia conducted a phase 3 clinical trial in order to assess if minimally invasive catheter evacuation of blood clots, followed by thrombolysis (with the aim of decreasing the clot size to 15 mL or less), could improve functional outcome in 242 patients (average age 62 years, 63% male) who underwent an intracerebral hemorrhage (ICH) event.
The procedure, called minimally invasive surgery plus alteplase for intracerebral hemorrhage evacuation (MISTIE) starts with computerized tomography (CT)-based navigation to develop a surgical approach plan, after which a rigid cannula is placed in the middle of the intracerebral blood clot. Surgeons then insert a soft drainage catheter, which facilitates up to nine injections of alteplase and passive clot removal. Evacuation is stopped when a hematoma size of 15 mL or less is achieved, as confirmed by daily CT scans.
Study results revealed that at one year, the proportion of patients with a modified Rankin Scale (mRS) score of 3 or less was not significantly higher in patients treated with the procedure (45%), compared to those who received standard medical care (41%). However, exploratory secondary analysis found that among the 58% of patients who had their hematoma reduced to a volume of 15 mL or less, there was a 10.5% difference in the likelihood of achieving a good functional outcome. The study was presented at the annual International Stroke Conference, held during January 2019 in Honolulu (Hawaii, USA).
“When assessing the results of surgery for brain hemorrhage, it is critical to consider how much blood was successfully evacuated. Unless a large majority of clot is removed and only a very small residual of blood is left, the full benefits of surgery will not be realized,” said senior author Professor Issam Awad, MD, MSc, of the University of Chicago. “This had never been considered as a factor in the success or failure of such surgeries, and cannot be taken for granted.”
Acute stroke due to supratentorial ICH is associated with high morbidity and mortality. Trials have not shown a benefit of hematoma evacuation with open craniotomy, and current guidelines have called for more evidence before making any recommendations about routine use of surgical interventions in this setting.
Related Links:
Johns Hopkins University
University of Chicago
Researchers at Johns Hopkins University (JHU; Baltimore, MD, USA), the University of Chicago (IL, USA), and 76 other hospitals in the USA, Canada, Europe, Australia, and Asia conducted a phase 3 clinical trial in order to assess if minimally invasive catheter evacuation of blood clots, followed by thrombolysis (with the aim of decreasing the clot size to 15 mL or less), could improve functional outcome in 242 patients (average age 62 years, 63% male) who underwent an intracerebral hemorrhage (ICH) event.
The procedure, called minimally invasive surgery plus alteplase for intracerebral hemorrhage evacuation (MISTIE) starts with computerized tomography (CT)-based navigation to develop a surgical approach plan, after which a rigid cannula is placed in the middle of the intracerebral blood clot. Surgeons then insert a soft drainage catheter, which facilitates up to nine injections of alteplase and passive clot removal. Evacuation is stopped when a hematoma size of 15 mL or less is achieved, as confirmed by daily CT scans.
Study results revealed that at one year, the proportion of patients with a modified Rankin Scale (mRS) score of 3 or less was not significantly higher in patients treated with the procedure (45%), compared to those who received standard medical care (41%). However, exploratory secondary analysis found that among the 58% of patients who had their hematoma reduced to a volume of 15 mL or less, there was a 10.5% difference in the likelihood of achieving a good functional outcome. The study was presented at the annual International Stroke Conference, held during January 2019 in Honolulu (Hawaii, USA).
“When assessing the results of surgery for brain hemorrhage, it is critical to consider how much blood was successfully evacuated. Unless a large majority of clot is removed and only a very small residual of blood is left, the full benefits of surgery will not be realized,” said senior author Professor Issam Awad, MD, MSc, of the University of Chicago. “This had never been considered as a factor in the success or failure of such surgeries, and cannot be taken for granted.”
Acute stroke due to supratentorial ICH is associated with high morbidity and mortality. Trials have not shown a benefit of hematoma evacuation with open craniotomy, and current guidelines have called for more evidence before making any recommendations about routine use of surgical interventions in this setting.
Related Links:
Johns Hopkins University
University of Chicago
Latest Critical Care News
- CPR Guidelines Updated for Pediatric and Neonatal Emergency Care and Resuscitation
- Ingestible Capsule Monitors Intestinal Inflammation
- Wireless Implantable Sensor Enables Continuous Endoleak Monitoring
- Pulse Oximeter Index Offers Non-Invasive Guides for Fluid Therapy
- Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
- 'Universal' Kidney to Match Any Blood Type
- Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
- AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
- Smartphone Imaging System Enables Early Oral Cancer Detection
- Swallowable Pill-Sized Bioprinter Treats GI Tract Injuries

- Personalized Brain “Pacemakers” Could Help Patients with Hard-To-Treat Epilepsy
- Microscopic DNA Flower Robots to Enable Precision Medicine Delivery
- Origami Robots to Deliver Medicine Less Invasively and More Effectively
- Improved Cough-Detection Technology Aids Health Monitoring
- AI Identifies Children in ER Likely to Develop Sepsis Within 48 Hours
- New Radiofrequency Therapy Slows Glioblastoma Growth
Channels
Critical Care
view channel
CPR Guidelines Updated for Pediatric and Neonatal Emergency Care and Resuscitation
Cardiac arrest in infants and children remains a leading cause of pediatric emergencies, with more than 7,000 out-of-hospital and 20,000 in-hospital cardiac arrests occurring annually in the United States.... Read more
Ingestible Capsule Monitors Intestinal Inflammation
Acute mesenteric ischemia—a life-threatening condition caused by blocked blood flow to the intestines—remains difficult to diagnose early because its symptoms often mimic common digestive problems.... Read more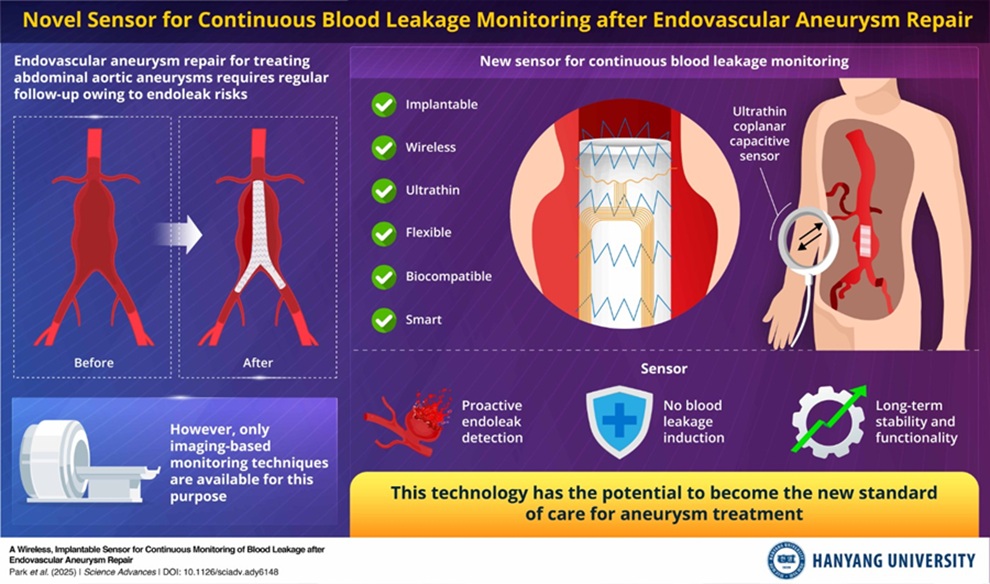
Wireless Implantable Sensor Enables Continuous Endoleak Monitoring
Endovascular aneurysm repair (EVAR) is a life-saving, minimally invasive treatment for abdominal aortic aneurysms—balloon-like bulges in the aorta that can rupture with fatal consequences.... Read more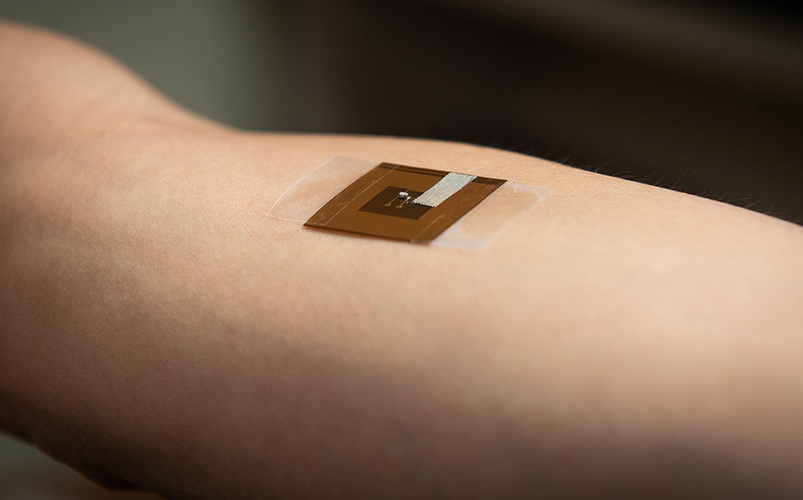
Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
Skin cancer remains one of the most dangerous and common cancers worldwide, with early detection crucial for improving survival rates. Traditional diagnostic methods—visual inspections, imaging, and biopsies—can... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more












