Heart Failure Sensor Cuts Hospitalizations in Half
|
By HospiMedica International staff writers Posted on 26 Mar 2019 |

Image: The implantable, battery-free CardioMEMS sensor (Photo courtesy of Abbott Vascular).
Heart failure (HF) patients show a 58% reduction in hospitalization after implantation of a pulmonary artery (PA) pressure measurement sensor, claims a new study.
The Abbott Vascular (Santa Clara, CA, USA) CardioMEMS Sensor is a permanently implantable wireless device that provides PA pressure measurements, including systolic, diastolic, and mean pressures, which can used to monitor cardiac status and initiate changes in medical therapy if necessary. The sensor consists of a resonant circuit that includes a capacitor and an induction coil; the capacitance is a function of pressure, and the resonant frequency is a function of capacitance. During the RF pulse, the sensor accumulates energy, which is re-radiated to an electronics unit that displays PA information as an 18 second waveform.
A study conducted by the University of Southern California (USC; Los Angeles, USA) showed that patients had an average of 0.52 HF hospitalizations in the year following implantation, compared to 1.24 before, regardless of the patients' ejection fraction. There were also benefits for females (61% reduction), blacks (53% reduction), patients with cardiac implantable electronic devices (CIEDs), and those with an ischemic or non-ischemic cardiomyopathy. The device also appeared to reduce all-cause hospitalizations for arrhythmias, pneumonia, and chronic obstructive pulmonary disease (COPD) by 28%.
CardioMEMS also met its safety endpoint, which was defined as freedom from device or system-related complications or sensor failure at one year post-implantation. Per the study data, only four patients experienced device- or system-related complications, and there was only one episode of sensor failure. The results translate into a 99.7% freedom from device/system-related complications and 99.9% freedom from sensor failure. The study was presented at the American College of Cardiology (ACC) 68th annual scientific session, held during March 2019 in New Orleans (LA, USA).
“If you can maintain more normal cardiac filling pressures and less heart stress, you are less likely to be seriously affected and need hospitalization for other conditions such as lung disease or liver disease, which are affected by heart function,” said lead author and study presenter David Shavelle, MD, of USC. “We believe that having the sensor monitored by their care team also encourages patients to follow their medication plan and gives them a sense of security that is particularly important for those living far away from a hospital.”
The Abbott Vascular (Santa Clara, CA, USA) CardioMEMS Sensor is a permanently implantable wireless device that provides PA pressure measurements, including systolic, diastolic, and mean pressures, which can used to monitor cardiac status and initiate changes in medical therapy if necessary. The sensor consists of a resonant circuit that includes a capacitor and an induction coil; the capacitance is a function of pressure, and the resonant frequency is a function of capacitance. During the RF pulse, the sensor accumulates energy, which is re-radiated to an electronics unit that displays PA information as an 18 second waveform.
A study conducted by the University of Southern California (USC; Los Angeles, USA) showed that patients had an average of 0.52 HF hospitalizations in the year following implantation, compared to 1.24 before, regardless of the patients' ejection fraction. There were also benefits for females (61% reduction), blacks (53% reduction), patients with cardiac implantable electronic devices (CIEDs), and those with an ischemic or non-ischemic cardiomyopathy. The device also appeared to reduce all-cause hospitalizations for arrhythmias, pneumonia, and chronic obstructive pulmonary disease (COPD) by 28%.
CardioMEMS also met its safety endpoint, which was defined as freedom from device or system-related complications or sensor failure at one year post-implantation. Per the study data, only four patients experienced device- or system-related complications, and there was only one episode of sensor failure. The results translate into a 99.7% freedom from device/system-related complications and 99.9% freedom from sensor failure. The study was presented at the American College of Cardiology (ACC) 68th annual scientific session, held during March 2019 in New Orleans (LA, USA).
“If you can maintain more normal cardiac filling pressures and less heart stress, you are less likely to be seriously affected and need hospitalization for other conditions such as lung disease or liver disease, which are affected by heart function,” said lead author and study presenter David Shavelle, MD, of USC. “We believe that having the sensor monitored by their care team also encourages patients to follow their medication plan and gives them a sense of security that is particularly important for those living far away from a hospital.”
Latest Critical Care News
- Smart Biosensors Could Be Game-Changer for Wearable Health Tech
- Low-Cost Medical Device Stops Postpartum Hemorrhages
- Non-Invasive Wearable Sensor Detects Sweat Biomarker in Low-Perspiration Conditions
- New Autoinjector Could Transform Trauma Care in Severe Bleeding Emergencies
- Portable Light-Based Brain Monitor Improves Dementia Diagnosis
- New Ultrasound Technique Enables Safer Vein Access in Critically Ill Patient
- CVD Risk Prediction Tool Could Guide Statin Therapy
- Wearables Could Revolutionize Pregnancy Monitoring and Detect Abnormalities
- AI Model Identifies AF Patients Requiring Blood Thinners to Prevent Stroke
- Soft Robot Intubation Device Could Save Lives
- Bee-Sting Inspired Wearable Microneedles to Revolutionize Drug Delivery
- Wearable Smart Patch Runs Tests Using Sweat Instead of Blood
- AI Improves Prediction of CKD Progression to End Stage Renal Disease
- First-Of-Its-Kind Online Tool to Revolutionize Treatment of High Blood Pressure
- Temperature-Sensing Patch Enables Early Breast Cancer Detection
- AI Stethoscope Detects Three Heart Conditions In 15 Seconds
Channels
Surgical Techniques
view channel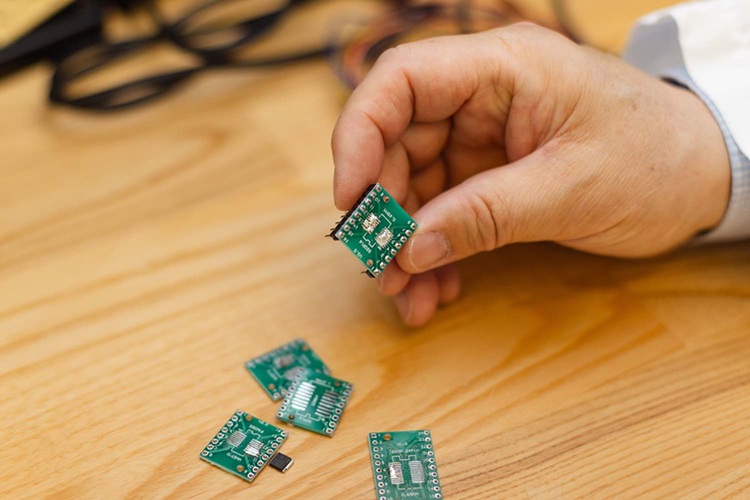
Micro Imaging Device Paired with Endoscope Spots Cancers at Earlier Stage
Digestive system cancers are among the most common cancers, with hundreds of thousands of new cases and deaths reported annually in the United States. Standard endoscopy, the main diagnostic method for... Read more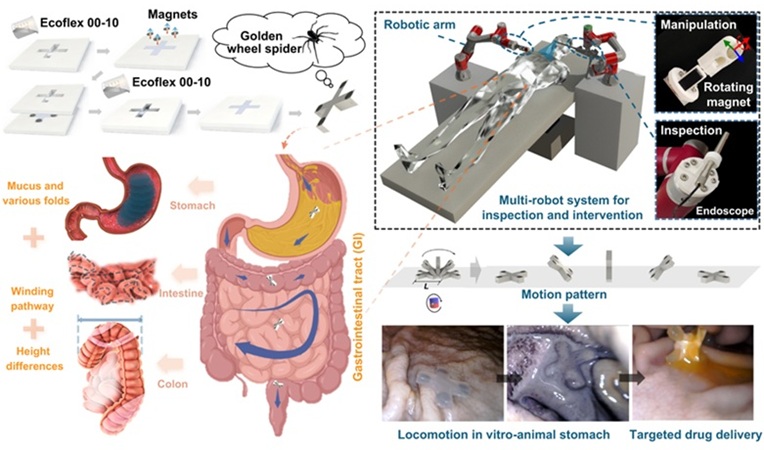
Spider-Inspired Magnetic Soft Robots to Perform Minimally Invasive GI Tract Procedures
The gastrointestinal (GI) tract is vital for digestion, nutrient absorption, and waste elimination, but it is also prone to cancers and other serious conditions. Standard endoscopy is widely used for diagnosis... Read more
AI Spine Model Could Reduce Surgical Risks
Nearly 3 in 10 adults in the United States have experienced lower back pain in any three months, making it the most common musculoskeletal pain. Back pain is one of the leading causes of disability worldwide,... Read more
Novel Method Uses Interstitial Fluid Flow to Predict Where Brain Tumor Can Grow Next
Glioblastoma is one of the most aggressive brain cancers, with patients surviving on average only 15 months after diagnosis. Surgery and radiation can temporarily control the tumor, but the disease almost... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more












