Biometric Toilet Seat Detects Congestive Heart Failure
|
By HospiMedica International staff writers Posted on 01 Apr 2019 |
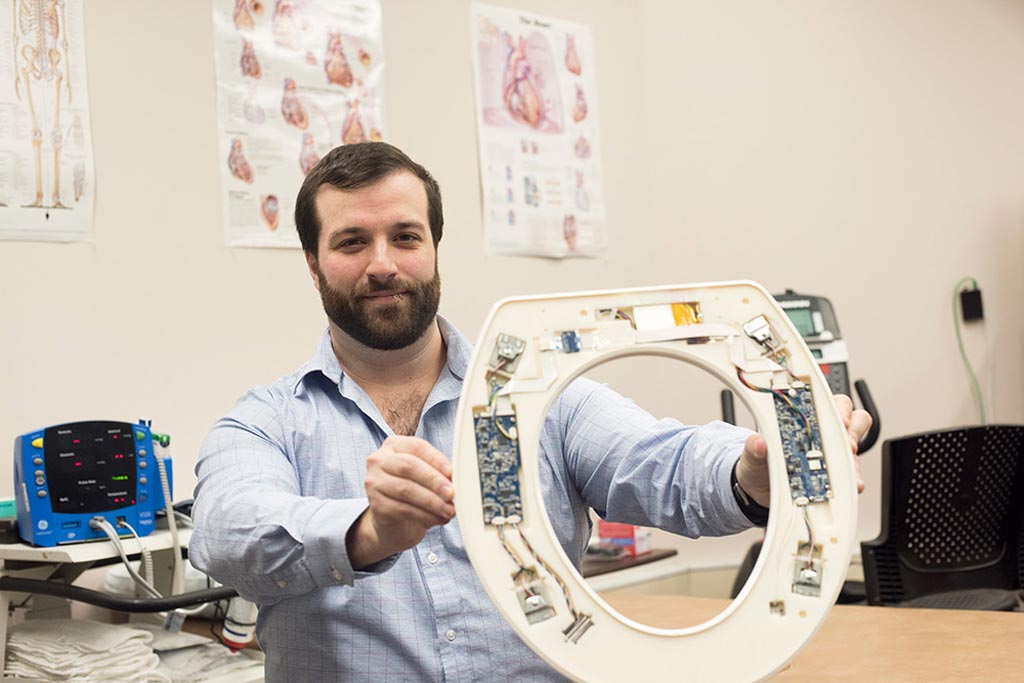
Image: Nicholas Conn presenting the toilet-seat based cardiovascular monitoring system (Photo courtesy of Sue Weisler/ RIT).
A toilet-seat based cardiovascular monitoring system can help lower hospital readmission rates for patients with congestive heart failure (CHF).
A product of Heart Health Intelligence (HHI; Rochester, NY, USA), the system integrates an electrocardiogram (ECG), ballistocardiogram (BCG), and photoplethysmogram (PPG) into a toilet seat capable of clinical-grade measurements of patient weight, pulse rate, systolic and diastolic blood pressure, stroke volume, and peripheral blood oxygenation. Software algorithms then analyze the data, alerting medical providers of a deteriorating condition. A report is also passed to hospital cardiologists, who can then determine if intervention is necessary.
The system installs directly on a standard toilet, is battery powered, wireless, waterproof, and requires no additional connections or user interaction, unobtrusively capturing cardiovascular data automatically whenever the user sits on the toilet. The seat incorporates a single-lead ECG for measuring the electrical activity of the heart and as a reference for ensemble averaging, a BCG for measuring the mechanical forces associated with the cardiac cycle, and a PPG for measuring SpO2 and pulse transit time (PTT). A floating hinge ensures that the weight on the seat is completely captured by the load cells, rather than having a portion of it carried by the hinge.
In a study that compared the toilet seat–based estimates of blood pressure and peripheral blood oxygenation to a hospital-grade vital signs monitor in 18 subjects over an eight-week period, clinical grade accuracy was achieved for all of measurements. Accuracy of diastolic and systolic blood pressure was 1.2 mm and –2.7 mm Hg, respectively. Stroke volume had an accuracy of –2.5 mL, compared to the gold standard, an echocardiogram (ECG). Peripheral blood oxygenation had an error of 2.3%. The study was published in the January 2019 issue of JMIR mHealth and uHealth.
“Typically, within 30 days of hospital discharge, 25% of patients with CHF are readmitted; after 90 days of hospital discharge, 45% of patients are readmitted,” said Nicholas Conn, PhD, founder and CEO of HHI and a researcher at the Rochester Institute of Technology (RIT; NY, USA). “The penalty alone for readmitting 150 patients is approximately USD 500,000 annually. The total cost of providing 150 patients with their own monitored toilet seats from HHI is USD 200,000. Hospital systems will save more than double their initial investment within one year.”
The U.S. Hospital Readmission Reduction Program (HRRP) was introduced by Medicare in order to improve patient care by penalizing hospitals with poor outcomes. One key outcome measure is the readmission rate; in 2013 Medicare levied fines of USD 227 million in fines against 2,225 hospitals that will have their payments reduced by up to 2% for a year. The penalties are based on readmissions of Medicare patients who originally went into the hospital with at least one of three conditions - heart attack, heart failure, and pneumonia.
Related Links:
Heart Health Intelligence
Rochester Institute of Technology
A product of Heart Health Intelligence (HHI; Rochester, NY, USA), the system integrates an electrocardiogram (ECG), ballistocardiogram (BCG), and photoplethysmogram (PPG) into a toilet seat capable of clinical-grade measurements of patient weight, pulse rate, systolic and diastolic blood pressure, stroke volume, and peripheral blood oxygenation. Software algorithms then analyze the data, alerting medical providers of a deteriorating condition. A report is also passed to hospital cardiologists, who can then determine if intervention is necessary.
The system installs directly on a standard toilet, is battery powered, wireless, waterproof, and requires no additional connections or user interaction, unobtrusively capturing cardiovascular data automatically whenever the user sits on the toilet. The seat incorporates a single-lead ECG for measuring the electrical activity of the heart and as a reference for ensemble averaging, a BCG for measuring the mechanical forces associated with the cardiac cycle, and a PPG for measuring SpO2 and pulse transit time (PTT). A floating hinge ensures that the weight on the seat is completely captured by the load cells, rather than having a portion of it carried by the hinge.
In a study that compared the toilet seat–based estimates of blood pressure and peripheral blood oxygenation to a hospital-grade vital signs monitor in 18 subjects over an eight-week period, clinical grade accuracy was achieved for all of measurements. Accuracy of diastolic and systolic blood pressure was 1.2 mm and –2.7 mm Hg, respectively. Stroke volume had an accuracy of –2.5 mL, compared to the gold standard, an echocardiogram (ECG). Peripheral blood oxygenation had an error of 2.3%. The study was published in the January 2019 issue of JMIR mHealth and uHealth.
“Typically, within 30 days of hospital discharge, 25% of patients with CHF are readmitted; after 90 days of hospital discharge, 45% of patients are readmitted,” said Nicholas Conn, PhD, founder and CEO of HHI and a researcher at the Rochester Institute of Technology (RIT; NY, USA). “The penalty alone for readmitting 150 patients is approximately USD 500,000 annually. The total cost of providing 150 patients with their own monitored toilet seats from HHI is USD 200,000. Hospital systems will save more than double their initial investment within one year.”
The U.S. Hospital Readmission Reduction Program (HRRP) was introduced by Medicare in order to improve patient care by penalizing hospitals with poor outcomes. One key outcome measure is the readmission rate; in 2013 Medicare levied fines of USD 227 million in fines against 2,225 hospitals that will have their payments reduced by up to 2% for a year. The penalties are based on readmissions of Medicare patients who originally went into the hospital with at least one of three conditions - heart attack, heart failure, and pneumonia.
Related Links:
Heart Health Intelligence
Rochester Institute of Technology
Channels
Critical Care
view channel
Magnetically Guided Microrobots to Enable Targeted Drug Delivery
Stroke affects 12 million people globally each year, often causing death or lasting disability. Current treatment relies on systemic administration of clot-dissolving drugs, which circulate throughout... Read more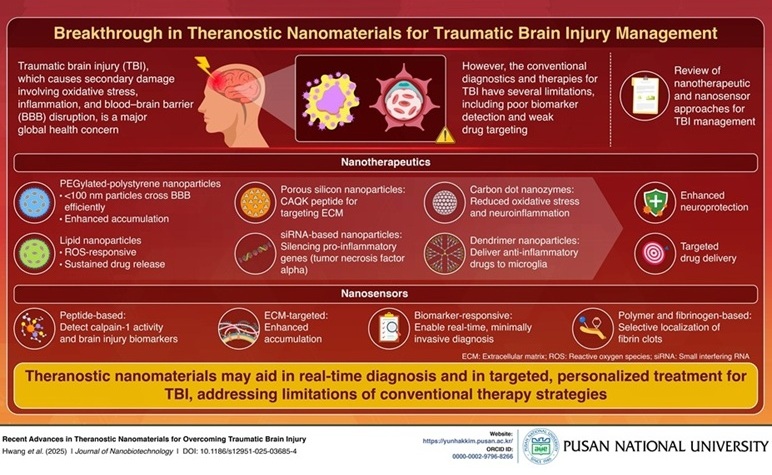
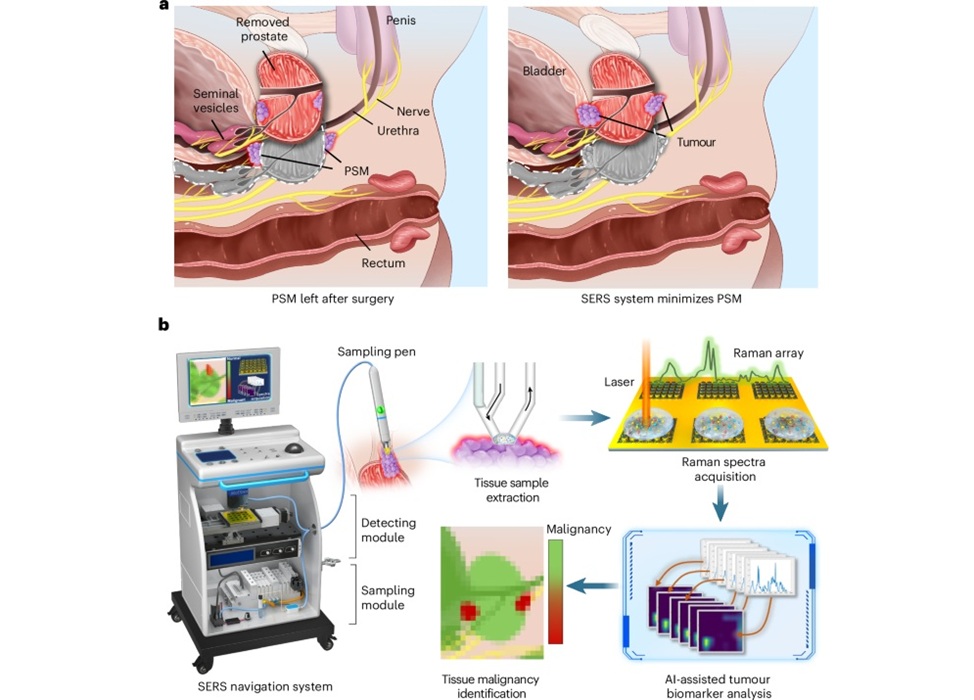
Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
Traumatic brain injury (TBI) continues to leave millions with long-term disabilities every year. After a sudden impact from a fall, collision, or accident, the brain undergoes inflammation, oxidative stress,... Read more
Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
Blood loss during or after surgery can place significant stress on people with heart disease, increasing the risk of dangerous complications. Transfusions are often delayed until hemoglobin levels fall... Read moreSurgical Techniques
view channel
New Study Findings Could Halve Number of Stent Procedures
When a coronary artery becomes acutely blocked during a heart attack, opening it immediately is essential to prevent irreversible damage. However, many patients also have other narrowed vessels that appear... Read more
Breakthrough Surgical Device Redefines Hip Arthroscopy
Hip arthroscopy has surged in popularity, yet surgeons still face major mechanical constraints when navigating deep joint spaces through traditional cannulas. Limited tool mobility and the need for an... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more