ICU Care Not Needed by Majority of Heart Attack Patients
|
By HospiMedica International staff writers Posted on 07 May 2019 |
Most patients who undergo ST-elevation myocardial infarction (STEMI) are at relatively low risk of developing a complication requiring intensive care unit (ICU) attention, according to a new study.
Researchers at the Duke Clinical Research Institute (DCRI; Durham, NC, USA), Virginia Commonwealth University (Richmond, USA), and other institutions conducted a study to examine variability in ICU utilization for patients with uncomplicated STEMI, evaluate the proportion of these patients who developed in-hospital complications requiring ICU care, and assess whether ICU use patterns and complication rates varied across categories of first medical contact to device times.
The patient population included 19,507 stable STEMI patients treated at 707 hospitals across the United States. The overall results of the study revealed that 82.3% of the patients were treated in an ICU with a median one-day stay period, but that only 16.2% of them subsequently developed complications that actually required ICU care while they were hospitalized. Of these, 3.7% died, 3.7% experienced cardiac arrest, 8.7% experienced shock, 0.9% suffered a stroke, 4.1% underwent atrioventricular block, and 5.7% experienced respiratory failure.
The study also found that patients who waited longer for treatment were more likely to develop at least one complication, not limited to a complication related to cardiac issues. Those who received treatment within an hour of being evaluated by emergency medical service (EMS) personnel or going directly to the hospital without being seen by EMS, had a complication rate of 13.4%, compared with an 18.7% rate for those who were not treated within 90 minutes. The study was published on April 15, 2019, in JACC: Cardiovascular Interventions.
“In the era of rapid primary percutaneous coronary intervention, ICUs may be overutilized, as patients presenting with STEMI are less likely to develop complications requiring ICU care,” concluded lead author cardiologist Jay Shavadia, MD, of DCRI, and colleagues. “Implementing a risk-based triage strategy, inclusive of factors such as degree of reperfusion delay, could optimize ICU utilization for patients with STEMI.”
STEMI occurs from the occlusion of one (or more) of the coronary arteries that supply the heart with blood. The cause of this abrupt disruption of blood flow is usually plaque rupture, erosion, fissuring, or dissection that results in an obstructing thrombus. STEMI is characterized by an ST-segment elevation as detected on a 12-lead electrocardiogram (ECG). Signs and symptoms include chest pain or discomfort, shortness of breath, dizziness or light-headedness, nausea or vomiting, diaphoresis (sweat), anxiety, and palpitations.
Related Links:
Duke Clinical Research Institute
Virginia Commonwealth University
Researchers at the Duke Clinical Research Institute (DCRI; Durham, NC, USA), Virginia Commonwealth University (Richmond, USA), and other institutions conducted a study to examine variability in ICU utilization for patients with uncomplicated STEMI, evaluate the proportion of these patients who developed in-hospital complications requiring ICU care, and assess whether ICU use patterns and complication rates varied across categories of first medical contact to device times.
The patient population included 19,507 stable STEMI patients treated at 707 hospitals across the United States. The overall results of the study revealed that 82.3% of the patients were treated in an ICU with a median one-day stay period, but that only 16.2% of them subsequently developed complications that actually required ICU care while they were hospitalized. Of these, 3.7% died, 3.7% experienced cardiac arrest, 8.7% experienced shock, 0.9% suffered a stroke, 4.1% underwent atrioventricular block, and 5.7% experienced respiratory failure.
The study also found that patients who waited longer for treatment were more likely to develop at least one complication, not limited to a complication related to cardiac issues. Those who received treatment within an hour of being evaluated by emergency medical service (EMS) personnel or going directly to the hospital without being seen by EMS, had a complication rate of 13.4%, compared with an 18.7% rate for those who were not treated within 90 minutes. The study was published on April 15, 2019, in JACC: Cardiovascular Interventions.
“In the era of rapid primary percutaneous coronary intervention, ICUs may be overutilized, as patients presenting with STEMI are less likely to develop complications requiring ICU care,” concluded lead author cardiologist Jay Shavadia, MD, of DCRI, and colleagues. “Implementing a risk-based triage strategy, inclusive of factors such as degree of reperfusion delay, could optimize ICU utilization for patients with STEMI.”
STEMI occurs from the occlusion of one (or more) of the coronary arteries that supply the heart with blood. The cause of this abrupt disruption of blood flow is usually plaque rupture, erosion, fissuring, or dissection that results in an obstructing thrombus. STEMI is characterized by an ST-segment elevation as detected on a 12-lead electrocardiogram (ECG). Signs and symptoms include chest pain or discomfort, shortness of breath, dizziness or light-headedness, nausea or vomiting, diaphoresis (sweat), anxiety, and palpitations.
Related Links:
Duke Clinical Research Institute
Virginia Commonwealth University
Latest Critical Care News
- Ingestible Capsule Monitors Intestinal Inflammation
- Wireless Implantable Sensor Enables Continuous Endoleak Monitoring
- Pulse Oximeter Index Offers Non-Invasive Guides for Fluid Therapy
- Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
- 'Universal' Kidney to Match Any Blood Type
- Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
- AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
- Smartphone Imaging System Enables Early Oral Cancer Detection
- Swallowable Pill-Sized Bioprinter Treats GI Tract Injuries

- Personalized Brain “Pacemakers” Could Help Patients with Hard-To-Treat Epilepsy
- Microscopic DNA Flower Robots to Enable Precision Medicine Delivery
- Origami Robots to Deliver Medicine Less Invasively and More Effectively
- Improved Cough-Detection Technology Aids Health Monitoring
- AI Identifies Children in ER Likely to Develop Sepsis Within 48 Hours
- New Radiofrequency Therapy Slows Glioblastoma Growth
- Battery-Free Wireless Multi-Sensing Platform Revolutionizes Pressure Injury Detection
Channels
Surgical Techniques
view channel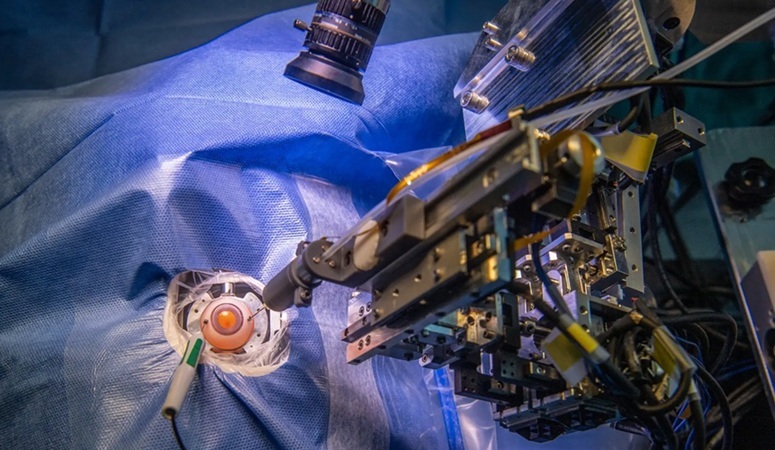
Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting nearly 200 million people, a figure expected to rise to 280 million by 2040. Current treatment involves doctors... Read more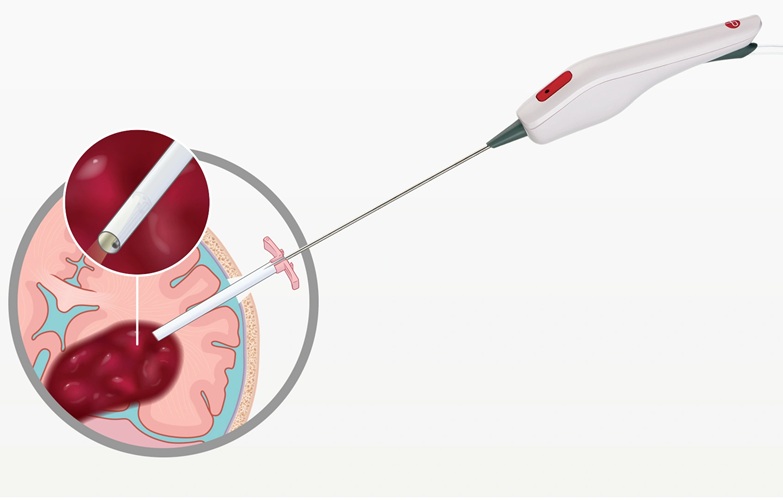
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more














