Surgical Safety Checklist Reduces Postoperative Mortality
|
By HospiMedica International staff writers Posted on 10 Jul 2019 |
Implementation of the World Health Organization (WHO; Geneva, Switzerland) Surgical Safety Checklist leads to a 37.2% reduction in inpatient postoperative mortality rates (POMR), claims a new study.
Researchers at the University of Birmingham (UB; United Kingdom) conducted a retrospective 16-year study of POMR (from 1998 to 2014) in England using data from the UK Hospital Episode Statistics and Office of National Statistics (HES-ONS) dataset. The results showed a general downward trend in POMR over the years, with a more than 30% relative reduction across all specialties, except colorectal oncology, cardiology, otorhinolaryngology, and plastic surgery. The greatest decrease was observed in the two years preceding WHO Surgical Safety Checklist implementation in 2008.
During the study period, there was an absolute POMR reduction of 0.71% per year, following which the annual pace of decrease fell. During the implementation and post-implementation periods, 10 of 14 specialties had a better than 5% relative reduction in POMRs; POMRs remained stable in plastic and cardiac surgery and increased in obstetrics and otorhinolaryngology. The greatest reductions occurred in esophagogastric (68.8%) and breast surgery (69.3%). The study was published on June 25, 2019, in the British Journal of Surgery.
“The improvements in postoperative mortality rates in Scotland and England could be replicated across low- and middle-income countries, but investment is urgently needed to identify and roll out successful strategies that improve surgical safety, including the WHO checklist, which is an important adjunct to making surgery safer,” concluded lead author Dmitri Nepogodiev, MBChB, of the UB National Institute for Health Research. “The checklist has been demonstrated to reduce POMR at an individual patient level, but this is the first evidence for its potential to improve outcomes at a national level.”
The WHO Surgical Safety Checklist is a 19-item checklist that identifies three distinct surgical phases, each corresponding to a specific period in the normal flow of work: Before the induction of anesthesia, before the initial incision, and before the patient leaves the operating facility. In each phase, a 'checklist coordinator' must confirm that the surgical team has completed the listed tasks before it proceeds with the procedure. The checklist is designed to systematically and efficiently ensure that all conditions are optimum for patient safety, all staff is identifiable and accountable, and errors in patient identity, site and type of procedure are avoided completely.
Related Links:
World Health Organization
University of Birmingham
Researchers at the University of Birmingham (UB; United Kingdom) conducted a retrospective 16-year study of POMR (from 1998 to 2014) in England using data from the UK Hospital Episode Statistics and Office of National Statistics (HES-ONS) dataset. The results showed a general downward trend in POMR over the years, with a more than 30% relative reduction across all specialties, except colorectal oncology, cardiology, otorhinolaryngology, and plastic surgery. The greatest decrease was observed in the two years preceding WHO Surgical Safety Checklist implementation in 2008.
During the study period, there was an absolute POMR reduction of 0.71% per year, following which the annual pace of decrease fell. During the implementation and post-implementation periods, 10 of 14 specialties had a better than 5% relative reduction in POMRs; POMRs remained stable in plastic and cardiac surgery and increased in obstetrics and otorhinolaryngology. The greatest reductions occurred in esophagogastric (68.8%) and breast surgery (69.3%). The study was published on June 25, 2019, in the British Journal of Surgery.
“The improvements in postoperative mortality rates in Scotland and England could be replicated across low- and middle-income countries, but investment is urgently needed to identify and roll out successful strategies that improve surgical safety, including the WHO checklist, which is an important adjunct to making surgery safer,” concluded lead author Dmitri Nepogodiev, MBChB, of the UB National Institute for Health Research. “The checklist has been demonstrated to reduce POMR at an individual patient level, but this is the first evidence for its potential to improve outcomes at a national level.”
The WHO Surgical Safety Checklist is a 19-item checklist that identifies three distinct surgical phases, each corresponding to a specific period in the normal flow of work: Before the induction of anesthesia, before the initial incision, and before the patient leaves the operating facility. In each phase, a 'checklist coordinator' must confirm that the surgical team has completed the listed tasks before it proceeds with the procedure. The checklist is designed to systematically and efficiently ensure that all conditions are optimum for patient safety, all staff is identifiable and accountable, and errors in patient identity, site and type of procedure are avoided completely.
Related Links:
World Health Organization
University of Birmingham
Latest Surgical Techniques News
- Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
- Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
- Novel Glue Prevents Complications After Breast Cancer Surgery
- Breakthrough Brain Implant Enables Safer and More Precise Drug Delivery
- Bioadhesive Sponge Stops Uncontrolled Internal Bleeding During Surgery
- Revolutionary Nano Bone Material to Accelerate Surgery and Healing
- Superior Orthopedic Implants Combat Infections and Quicken Healing After Surgery
- Laser-Based Technique Eliminates Pancreatic Tumors While Protecting Healthy Tissue
- Surgical Treatment of Severe Carotid Artery Stenosis Benefits Blood-Brain Barrier
- Revolutionary Reusable Duodenoscope Introduces 68-Minute Sterilization
- World's First Transcatheter Smart Implant Monitors and Treats Congestion in Heart Failure
- Hybrid Endoscope Marks Breakthrough in Surgical Visualization
- Robot-Assisted Bronchoscope Diagnoses Tiniest and Hardest to Reach Lung Tumors
- Diamond-Titanium Device Paves Way for Smart Implants that Warn of Disease Progression
- 3D Printable Bio-Active Glass Could Serve as Bone Replacement Material
- Spider-Inspired Magnetic Soft Robots to Perform Minimally Invasive GI Tract Procedures
Channels
Critical Care
view channel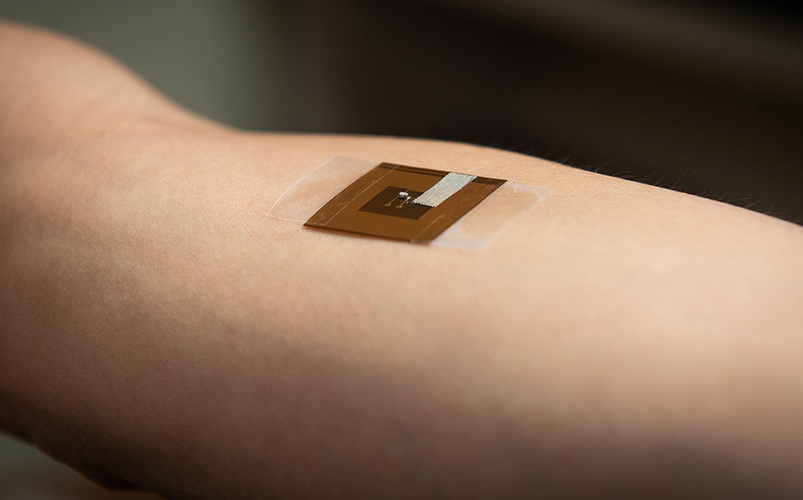
Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
Skin cancer remains one of the most dangerous and common cancers worldwide, with early detection crucial for improving survival rates. Traditional diagnostic methods—visual inspections, imaging, and biopsies—can... Read more
Pulse Oximeter Index Offers Non-Invasive Guides for Fluid Therapy
In patients with acute circulatory failure, deciding whether to administer intravenous fluids is often a life-or-death decision. Too little fluid can leave organs underperfused, while too much can cause... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more