Machine Learning Approach Predicts Surgery Duration
|
By HospiMedica International staff writers Posted on 01 Aug 2019 |
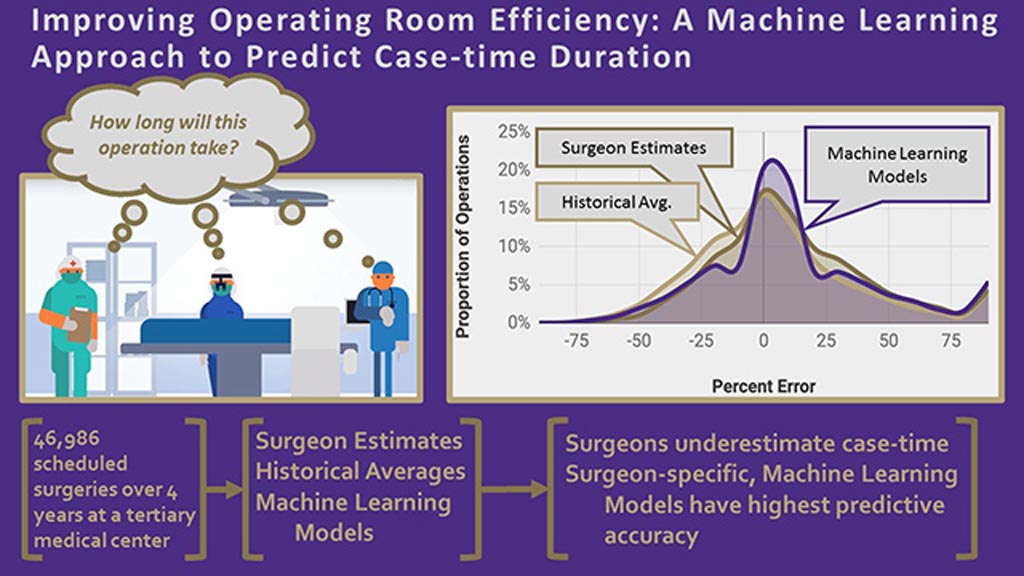
Image: A graphical abstract of the OR AI algorithm (Photo courtesy of UW).
A novel artificial intelligence (AI) based statistical model uses large retrospective datasets to improve estimation of surgical procedures duration.
Researchers at the University of Washington (UW; Seattle, USA) and Perimatics (Bellevue, WA, USA) used a dataset that included 46,986 scheduled surgeries performed by 92 surgeons at UW between January 2014 and December 2017 in order to develop, test, and train machine learning (ML) statistical models that could improve operating room (OR) efficiency by better predicting case-time duration. The models were developed on a training dataset that included 80% of the dataset, and validated on a testing dataset of the remaining 20%.
The predictions derived by ML were then compared to average historical procedure times and surgeon estimates, with individual models created for each surgical service and surgeon, respectively. The results showed that the ML algorithm could predict case times within a 10% threshold. Surgeon-specific models were able to improve accuracy from 30% (based on a surgeon's estimate) to 39%, and among the top one-third of surgeons, accuracy improved to more than 50%. The study was published on July 18, 2019, in the Journal of the American College of Surgeons (JACS).
“OR scheduling is a five billion dollar problem. To optimize the OR, you have to answer a fundamental question: How long does each surgery take? Underutilization means fewer patients get surgical care and the hospital has excess capacity. Overutilization results in cancelled operations and overtime expenses,” said study co-lead author Rajeev Saxena, MD, of the UW School of Medicine. “You can change an entire organizational culture by taking a data-forward approach and engaging key stakeholders.”
Many variables need to be considered when attempting to optimize surgical scheduling, including case duration, patient waiting time for surgery, and the number of blocks of OR time given to each surgeon or surgical service, as determined by OR committees. A utilization threshold of 75% is appropriate for most ORs, but if a hospital can strengthen OR utilization, it can grow revenue by increasing total case volume.
Related Links:
University of Washington
Perimatics
Researchers at the University of Washington (UW; Seattle, USA) and Perimatics (Bellevue, WA, USA) used a dataset that included 46,986 scheduled surgeries performed by 92 surgeons at UW between January 2014 and December 2017 in order to develop, test, and train machine learning (ML) statistical models that could improve operating room (OR) efficiency by better predicting case-time duration. The models were developed on a training dataset that included 80% of the dataset, and validated on a testing dataset of the remaining 20%.
The predictions derived by ML were then compared to average historical procedure times and surgeon estimates, with individual models created for each surgical service and surgeon, respectively. The results showed that the ML algorithm could predict case times within a 10% threshold. Surgeon-specific models were able to improve accuracy from 30% (based on a surgeon's estimate) to 39%, and among the top one-third of surgeons, accuracy improved to more than 50%. The study was published on July 18, 2019, in the Journal of the American College of Surgeons (JACS).
“OR scheduling is a five billion dollar problem. To optimize the OR, you have to answer a fundamental question: How long does each surgery take? Underutilization means fewer patients get surgical care and the hospital has excess capacity. Overutilization results in cancelled operations and overtime expenses,” said study co-lead author Rajeev Saxena, MD, of the UW School of Medicine. “You can change an entire organizational culture by taking a data-forward approach and engaging key stakeholders.”
Many variables need to be considered when attempting to optimize surgical scheduling, including case duration, patient waiting time for surgery, and the number of blocks of OR time given to each surgeon or surgical service, as determined by OR committees. A utilization threshold of 75% is appropriate for most ORs, but if a hospital can strengthen OR utilization, it can grow revenue by increasing total case volume.
Related Links:
University of Washington
Perimatics
Latest AI News
Channels
Critical Care
view channel
Origami Robots to Deliver Medicine Less Invasively and More Effectively
Delivering medicine to ulcers or other internal sites often requires invasive procedures that can disrupt surrounding tissues and lengthen recovery times. Traditional magnetic actuators used in soft robotics... Read more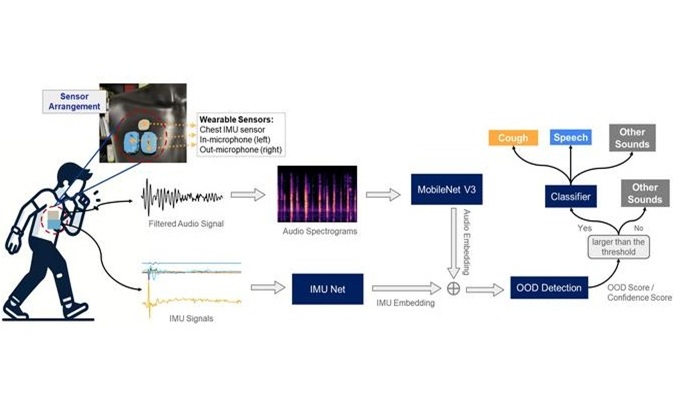
Improved Cough-Detection Technology Aids Health Monitoring
Coughing serves as an important biomarker for tracking a variety of conditions and can help monitor the progress of respiratory diseases or predict when someone’s asthma is being exacerbated.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more














