Wireless-Controlled Soft Neural Implant Stimulates Brain Cells
|
By HospiMedica International staff writers Posted on 22 Aug 2019 |
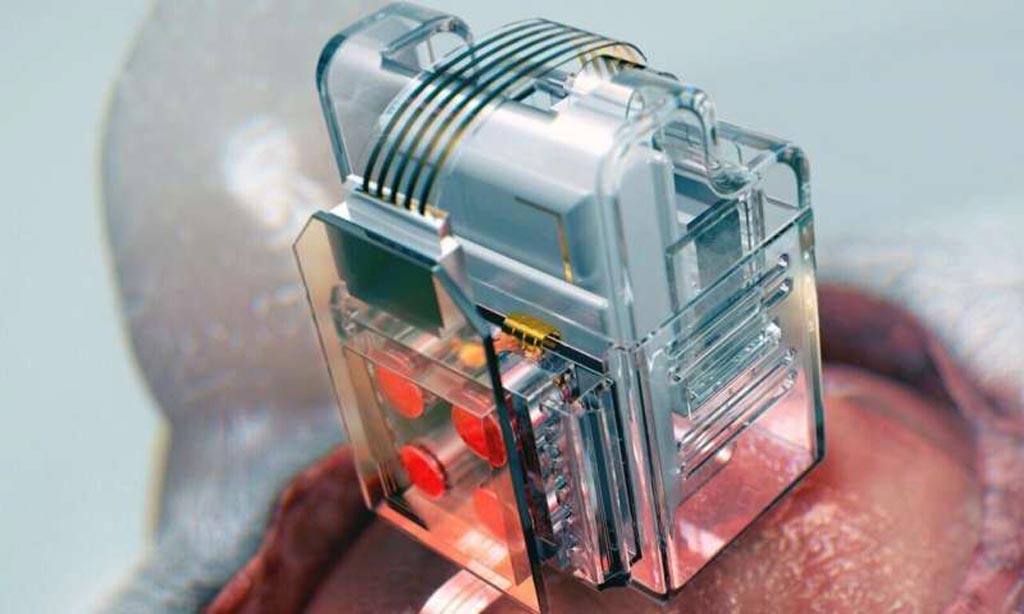
Image: Lego-like replaceable drug cartridges and LEDs help target specific neurons of interest (Photo courtesy of KAIST).
A soft neural implant operated by a smartphone can deliver multiple drugs and colored light to control Parkinson's, Alzheimer's, addiction, depression, and pain, according to a new study.
Developed at the Korea Advanced Institute of Science and Technology (KAIST; Daejeon, Republic of Korea), the University of Washington (UW; Seattle, USA) and the University of Colorado (Boulder, USA), the neural implant includes a soft, ultrathin probe (the thickness of a human hair), which holds microfluidic channels and tiny LEDs, smaller than a grain of salt. The implant also holds 'plug-n-play' replaceable drug cartridges, which allows continuous neuropharmacology and photostimulation of the same brain circuits with unlimited drug doses and light delivery.
Activation of the wireless implantable optofluidic brain probe is controlled with a simple user interface on any smartphone, providing neuroscientists with the ability to easily trigger any specific combination or precise sequencing of LED light and drug delivery, without being physically inside the laboratory, and even set up fully automated delivery. For the study, the researchers demonstrated the use of the probes by controlling locomotor activity in mice for over four weeks. The study was published on August 5, 2019, in Nature Biomedical Engineering.
“This technology significantly overshadows the conventional methods used by neuroscientists, which usually involve rigid metal tubes and optical fibers to deliver drugs and light,” said lead author Raza Qazi, PhD, of KAIST and University of Colorado Boulder. “Apart from limiting the subject's movement due to bulky equipment, their relatively rigid structure causes lesions in soft brain tissue over time, therefore making them not suitable for long-term implantation. We are interested in further developing this technology to make a brain implant for clinical applications.”
“This technology will help researchers in many ways. It allows us to better dissect the neural circuit basis of behavior, and how specific neuromodulators in the brain tune behavior in various ways,” added senior study co-author professor of anesthesiology, pain medicine, and pharmacology Michael Bruchas, MD, PhD, of the UW School of Medicine. “We are also eager to use the device for complex pharmacological studies, which could help us develop new therapeutics for pain, addiction, and emotional disorders.”
Photostimulation is the use of light to artificially activate biological compounds, cells, tissues or even whole organisms. One form of photostimulation is optogenetics, which has shown significant promise in the treatment of a series of neurological disorders such as Parkinson’s disease and epilepsy by targeting specific cell types or neural circuits. So far, it has only been implemented for research purposes in the field of neurobiology, serving to reveal more about the mechanisms of specific disorders.
Related Links:
Korea Advanced Institute of Science and Technology
University of Washington
University of Colorado
Developed at the Korea Advanced Institute of Science and Technology (KAIST; Daejeon, Republic of Korea), the University of Washington (UW; Seattle, USA) and the University of Colorado (Boulder, USA), the neural implant includes a soft, ultrathin probe (the thickness of a human hair), which holds microfluidic channels and tiny LEDs, smaller than a grain of salt. The implant also holds 'plug-n-play' replaceable drug cartridges, which allows continuous neuropharmacology and photostimulation of the same brain circuits with unlimited drug doses and light delivery.
Activation of the wireless implantable optofluidic brain probe is controlled with a simple user interface on any smartphone, providing neuroscientists with the ability to easily trigger any specific combination or precise sequencing of LED light and drug delivery, without being physically inside the laboratory, and even set up fully automated delivery. For the study, the researchers demonstrated the use of the probes by controlling locomotor activity in mice for over four weeks. The study was published on August 5, 2019, in Nature Biomedical Engineering.
“This technology significantly overshadows the conventional methods used by neuroscientists, which usually involve rigid metal tubes and optical fibers to deliver drugs and light,” said lead author Raza Qazi, PhD, of KAIST and University of Colorado Boulder. “Apart from limiting the subject's movement due to bulky equipment, their relatively rigid structure causes lesions in soft brain tissue over time, therefore making them not suitable for long-term implantation. We are interested in further developing this technology to make a brain implant for clinical applications.”
“This technology will help researchers in many ways. It allows us to better dissect the neural circuit basis of behavior, and how specific neuromodulators in the brain tune behavior in various ways,” added senior study co-author professor of anesthesiology, pain medicine, and pharmacology Michael Bruchas, MD, PhD, of the UW School of Medicine. “We are also eager to use the device for complex pharmacological studies, which could help us develop new therapeutics for pain, addiction, and emotional disorders.”
Photostimulation is the use of light to artificially activate biological compounds, cells, tissues or even whole organisms. One form of photostimulation is optogenetics, which has shown significant promise in the treatment of a series of neurological disorders such as Parkinson’s disease and epilepsy by targeting specific cell types or neural circuits. So far, it has only been implemented for research purposes in the field of neurobiology, serving to reveal more about the mechanisms of specific disorders.
Related Links:
Korea Advanced Institute of Science and Technology
University of Washington
University of Colorado
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read moreSurgical Techniques
view channel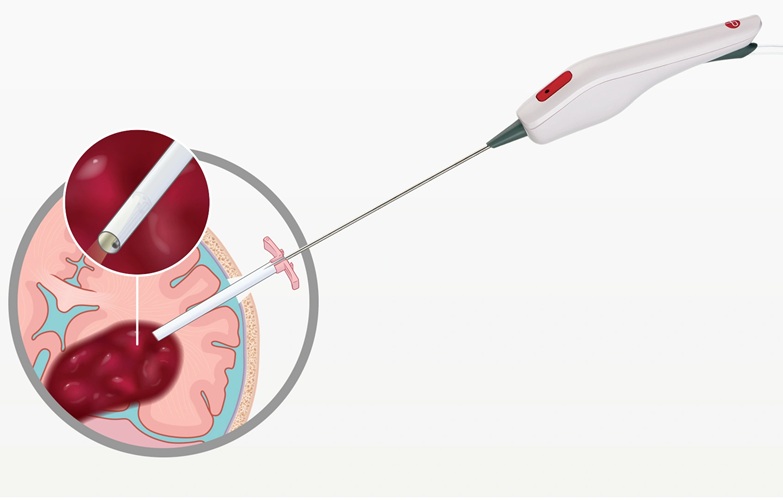
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more