Wound Closure System Outperforms Staples and Sutures
|
By HospiMedica International staff writers Posted on 06 Sep 2019 |
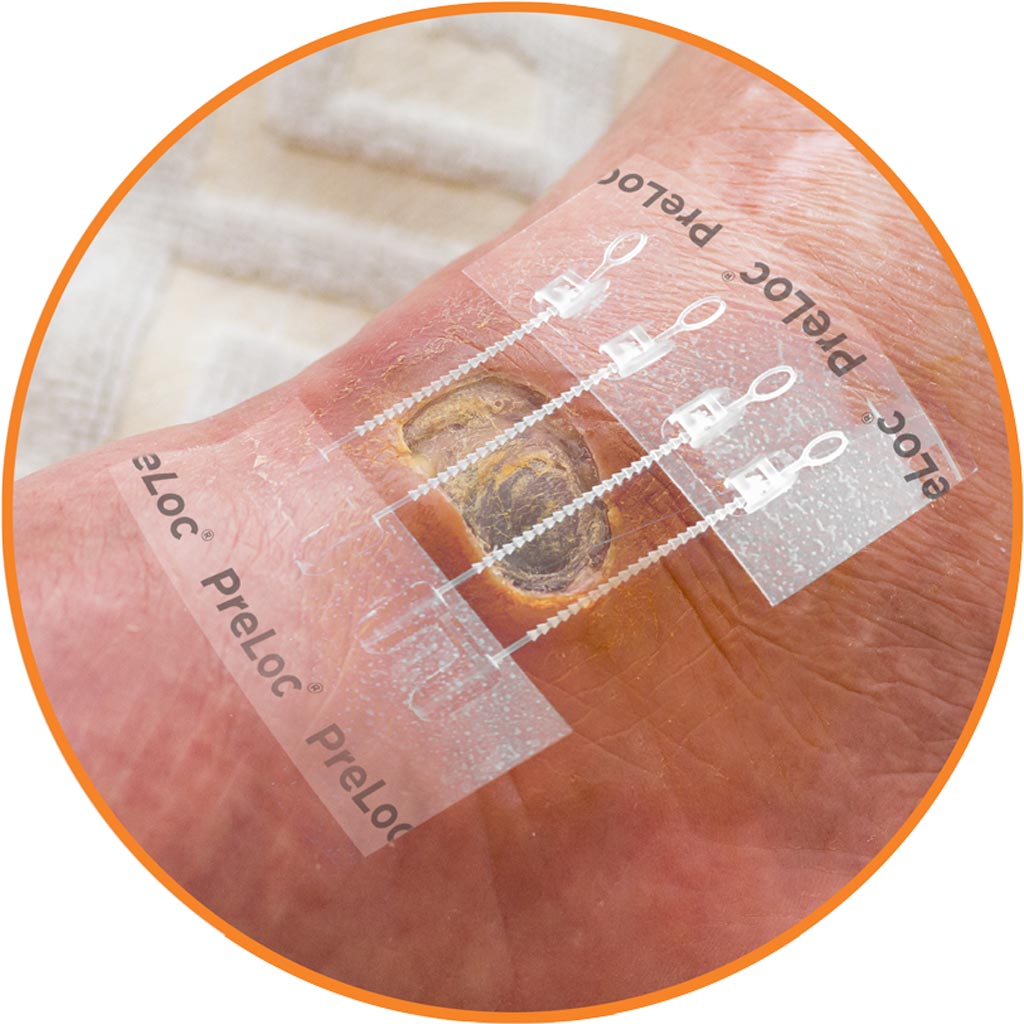
Image: The Preloc monofilament base before wound closure (Photo courtesy of Zipline Medical).
A novel skin closure system reduces incision-related problems, provides greater range of motion, reduces pain, and results in superior scar quality.
The ZipLine Medical (Campbell, CA, USA) Pre-placement RE-aligning LOw-tension Closure (PRELOC) system is a non-invasive and easy-to-use skin closure device that replaces sutures, staples, and glue for surgical incisions and lacerations. A breathable monofilm base, which is applied before the incision, facilitates re-approximation of incision edges. Once the zipped tags are pulled, tension in the surrounding skin is bridged over and around the incision, resulting in a low-tension and uniform distribution of closure forces, unlike point load forces typical of staples and sutures.
And since no skin piercing is involved, there is a reduced risk of surgical site infection (SSI) and needle stick injury. The transparent materials facilitate monitoring of the area surrounding the incision, as well as supporting retraction for access and visualization of the surgical site. After the incision has healed, the device is easily removed by simply peeling it off from the skin; no extra instruments or special skills are required, reducing the need for an additional patient return visit for staple or suture removal.
In a health economics retrospective chart review study conducted in 130 total knee replacement (TKR) patients, those receiving staples had more incision-related phone calls to the clinic, incision-related emergency room (ER) admissions, incision-related clinic visits, and antibiotics prescribed due to complications than the patients with the Zip closure device. The clinic cost for a problem staple patient was almost double that of the Zip group, while the opportunity cost for a problem staple patient was quadruple that of the Zip group (USD 228 versus USD 50, respectively). The study was published on March 20, 2019, in Cureus.
“The results of this study provide insight on how a simple change in the closure methodology can lead to potential downstream cost savings, especially in a bundled payment model,” said lead author Roger Emerson, MD, of the Texas Center for Joint Replacement (Plano, TX, USA). “Patients were apprehensive about staple removal and concerned when they saw redness around their staples, which in some cases triggered antibiotic prescriptions to avoid possible infection.”
Related Links:
ZipLine Medical
The ZipLine Medical (Campbell, CA, USA) Pre-placement RE-aligning LOw-tension Closure (PRELOC) system is a non-invasive and easy-to-use skin closure device that replaces sutures, staples, and glue for surgical incisions and lacerations. A breathable monofilm base, which is applied before the incision, facilitates re-approximation of incision edges. Once the zipped tags are pulled, tension in the surrounding skin is bridged over and around the incision, resulting in a low-tension and uniform distribution of closure forces, unlike point load forces typical of staples and sutures.
And since no skin piercing is involved, there is a reduced risk of surgical site infection (SSI) and needle stick injury. The transparent materials facilitate monitoring of the area surrounding the incision, as well as supporting retraction for access and visualization of the surgical site. After the incision has healed, the device is easily removed by simply peeling it off from the skin; no extra instruments or special skills are required, reducing the need for an additional patient return visit for staple or suture removal.
In a health economics retrospective chart review study conducted in 130 total knee replacement (TKR) patients, those receiving staples had more incision-related phone calls to the clinic, incision-related emergency room (ER) admissions, incision-related clinic visits, and antibiotics prescribed due to complications than the patients with the Zip closure device. The clinic cost for a problem staple patient was almost double that of the Zip group, while the opportunity cost for a problem staple patient was quadruple that of the Zip group (USD 228 versus USD 50, respectively). The study was published on March 20, 2019, in Cureus.
“The results of this study provide insight on how a simple change in the closure methodology can lead to potential downstream cost savings, especially in a bundled payment model,” said lead author Roger Emerson, MD, of the Texas Center for Joint Replacement (Plano, TX, USA). “Patients were apprehensive about staple removal and concerned when they saw redness around their staples, which in some cases triggered antibiotic prescriptions to avoid possible infection.”
Related Links:
ZipLine Medical
Latest Surgical Techniques News
- Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
- Novel Glue Prevents Complications After Breast Cancer Surgery
- Breakthrough Brain Implant Enables Safer and More Precise Drug Delivery
- Bioadhesive Sponge Stops Uncontrolled Internal Bleeding During Surgery
- Revolutionary Nano Bone Material to Accelerate Surgery and Healing
- Superior Orthopedic Implants Combat Infections and Quicken Healing After Surgery
- Laser-Based Technique Eliminates Pancreatic Tumors While Protecting Healthy Tissue
- Surgical Treatment of Severe Carotid Artery Stenosis Benefits Blood-Brain Barrier
- Revolutionary Reusable Duodenoscope Introduces 68-Minute Sterilization
- World's First Transcatheter Smart Implant Monitors and Treats Congestion in Heart Failure
- Hybrid Endoscope Marks Breakthrough in Surgical Visualization
- Robot-Assisted Bronchoscope Diagnoses Tiniest and Hardest to Reach Lung Tumors
- Diamond-Titanium Device Paves Way for Smart Implants that Warn of Disease Progression
- 3D Printable Bio-Active Glass Could Serve as Bone Replacement Material
- Spider-Inspired Magnetic Soft Robots to Perform Minimally Invasive GI Tract Procedures
- Micro Imaging Device Paired with Endoscope Spots Cancers at Earlier Stage
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more