Artificial Intelligence Accurately Predicts Radiation Treatment Side Effects
|
By HospiMedica International staff writers Posted on 01 Oct 2019 |

Image: New research has shown that a computer model can predict side effects associated with radiation therapy (Photo courtesy of Technology Networks).
Researchers from the University of Texas MD Anderson Cancer Center (Houston, Texas, USA) have demonstrated that a sophisticated computer model can accurately predict two of the most challenging side effects associated with radiation therapy for head and neck cancer. This precision oncology approach has the potential to better identify patients who might benefit from early interventions that could help prevent significant weight loss after treatment or reduce the need for feeding tube placement.
The team of researchers developed models to analyze large sets of data merged from three sources: electronic health records (Epic), an internal web-based charting tool (Brocade) and the record/verify system (Mosaiq). The data included more than 700 clinical and treatment variables for patients with head and neck cancer (75% male/25% female, with a median age of 62 years) who received more than 2,000 courses of radiation therapy (median dose 60 Gy) across five practice sites at MD Anderson from 2016 to 2018.
The researchers used the models to predict three endpoints: significant weight loss, feeding tube placement and unplanned hospitalizations. Results from the best-performing model were then validated against 225 subsequent consecutive radiation therapy treatments. Models with a performance rate that met a pre-specified threshold of area under the curve (AUC) of 0.70 or higher were considered clinically valid (an AUC score of 1.0 would mean the model’s predictions were 100% accurate, while a score of 0.0 would mean the predictions were never accurate). The models predicted the likelihood of significant weight loss (AUC = 0.751) and need for feeding tube placement (AUC = 0.755) with a high degree of accuracy.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center and lead author on the study. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
The machine learning approach cannot isolate the single-most predictive factor or combination of factors that lead to negative side effects, but can provide patients and their clinicians with a better understanding of what to expect during the course of treatment. In addition to predicting the likelihood of side effects, machine learning models could potentially predict which treatment plans would be most effective for different types of patients and allow for more personalized approaches to radiation oncology.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” added Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
Related Links:
University of Texas MD Anderson Cancer Center
The team of researchers developed models to analyze large sets of data merged from three sources: electronic health records (Epic), an internal web-based charting tool (Brocade) and the record/verify system (Mosaiq). The data included more than 700 clinical and treatment variables for patients with head and neck cancer (75% male/25% female, with a median age of 62 years) who received more than 2,000 courses of radiation therapy (median dose 60 Gy) across five practice sites at MD Anderson from 2016 to 2018.
The researchers used the models to predict three endpoints: significant weight loss, feeding tube placement and unplanned hospitalizations. Results from the best-performing model were then validated against 225 subsequent consecutive radiation therapy treatments. Models with a performance rate that met a pre-specified threshold of area under the curve (AUC) of 0.70 or higher were considered clinically valid (an AUC score of 1.0 would mean the model’s predictions were 100% accurate, while a score of 0.0 would mean the predictions were never accurate). The models predicted the likelihood of significant weight loss (AUC = 0.751) and need for feeding tube placement (AUC = 0.755) with a high degree of accuracy.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center and lead author on the study. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
The machine learning approach cannot isolate the single-most predictive factor or combination of factors that lead to negative side effects, but can provide patients and their clinicians with a better understanding of what to expect during the course of treatment. In addition to predicting the likelihood of side effects, machine learning models could potentially predict which treatment plans would be most effective for different types of patients and allow for more personalized approaches to radiation oncology.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” added Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
Related Links:
University of Texas MD Anderson Cancer Center
Latest AI News
Channels
Critical Care
view channel
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read more
AI Heart Attack Risk Assessment Tool Outperforms Existing Methods
For decades, doctors have relied on standardized scoring systems to assess patients with the most common type of heart attack—non-ST-elevation acute coronary syndrome (NSTE-ACS). The GRACE score, used... Read moreSurgical Techniques
view channel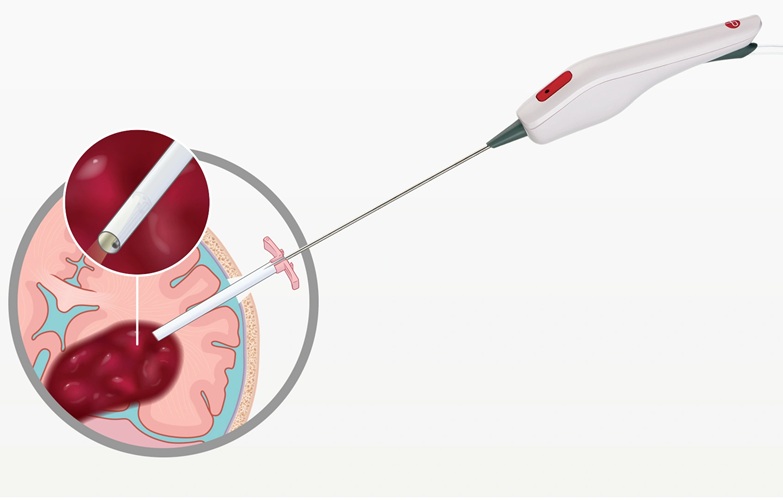
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read more
Novel Glue Prevents Complications After Breast Cancer Surgery
Seroma and prolonged lymphorrhea are among the most common complications following axillary lymphadenectomy in breast cancer patients. These postoperative issues can delay recovery and postpone the start... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more