Headache after Childbirth Epidural Could Indicate Subdural Hematoma
|
By HospiMedica International staff writers Posted on 29 Oct 2019 |
Women who experience headaches following neuraxial anesthesia prior to giving birth have a greater risk of developing intracranial subdural hematoma (ISH), according to a new study.
Researchers at McGill University (Montreal, Canada) and the University of Toronto (UT; Canada) reviewed the outcomes of 22,130,815 patients and deliveries in the United States between January 2010 and December 2016 in order to determine the association of post–dural puncture headache with postpartum ISH. Patients were included if they had two months of follow-up data, and did not receive a diagnostic lumbar puncture. The main outcome was ISH in the two-month postpartum period, with secondary outcomes including in-hospital mortality and occurrence of neurosurgery.
In all, there were 68,374 post–dural puncture headaches, for an overall rate of 309 per 100,000. There were 342 cases of ISH identified, indicating an incidence rate of 1.5 per 100,000 women. Of these, 100 cases were in women with post–dural puncture headache, indicating a rate of 147 hematoma cases per 100,000 deliveries in this subgroup. After adjustment for maternal age, cesarean delivery, hypertension, preeclampsia, and other co-morbidities, post–dural puncture headache had an odds ratio for subdural hematoma of 199, and an adjusted absolute risk increase of 130 per 100,000 deliveries. The study was published on September 16, 2019, in JAMA Neurology.
“When a patient has a post-dural puncture headache, they are at risk for a subdural hematoma, which can result in serious morbidity and increased mortality, and needs to be considered by any clinician looking after these patients,” said lead author Albert Moore, MD, of McGill University. “The risk is higher in patients who have coagulopathy, previous cerebral arteriovenous malformations, and hypertensive disease, and there is also a possibility that delaying a blood patch may increase the risk of developing a subdural hematoma.”
Post–dural puncture headache is thought to be caused by decreased intracranial pressure attributable to the leakage of cerebrospinal fluid (CSF) through the dural disruption, which places traction on pain-sensitive structures. Treatment often involves a blood patch, which is the injection of autologous whole blood into the epidural space. As pregnant women frequently receive neuraxial anesthesia for childbirth, they may develop symptoms of a post–dural puncture headache after their hospital discharge.
Related Links:
McGill University
University of Toronto
Researchers at McGill University (Montreal, Canada) and the University of Toronto (UT; Canada) reviewed the outcomes of 22,130,815 patients and deliveries in the United States between January 2010 and December 2016 in order to determine the association of post–dural puncture headache with postpartum ISH. Patients were included if they had two months of follow-up data, and did not receive a diagnostic lumbar puncture. The main outcome was ISH in the two-month postpartum period, with secondary outcomes including in-hospital mortality and occurrence of neurosurgery.
In all, there were 68,374 post–dural puncture headaches, for an overall rate of 309 per 100,000. There were 342 cases of ISH identified, indicating an incidence rate of 1.5 per 100,000 women. Of these, 100 cases were in women with post–dural puncture headache, indicating a rate of 147 hematoma cases per 100,000 deliveries in this subgroup. After adjustment for maternal age, cesarean delivery, hypertension, preeclampsia, and other co-morbidities, post–dural puncture headache had an odds ratio for subdural hematoma of 199, and an adjusted absolute risk increase of 130 per 100,000 deliveries. The study was published on September 16, 2019, in JAMA Neurology.
“When a patient has a post-dural puncture headache, they are at risk for a subdural hematoma, which can result in serious morbidity and increased mortality, and needs to be considered by any clinician looking after these patients,” said lead author Albert Moore, MD, of McGill University. “The risk is higher in patients who have coagulopathy, previous cerebral arteriovenous malformations, and hypertensive disease, and there is also a possibility that delaying a blood patch may increase the risk of developing a subdural hematoma.”
Post–dural puncture headache is thought to be caused by decreased intracranial pressure attributable to the leakage of cerebrospinal fluid (CSF) through the dural disruption, which places traction on pain-sensitive structures. Treatment often involves a blood patch, which is the injection of autologous whole blood into the epidural space. As pregnant women frequently receive neuraxial anesthesia for childbirth, they may develop symptoms of a post–dural puncture headache after their hospital discharge.
Related Links:
McGill University
University of Toronto
Latest Critical Care News
- New Inhalable Treatment for TB Lowers Side Effects
- AI Algorithm Improves Antibiotic Decision-Making in Urinary Tract Infection
- 3D-Printed System Enhances Vaccine Delivery Via Microneedle Array Patch
- Whole-Heart Mapping Technology Provides Comprehensive Real-Time View of Arrhythmias
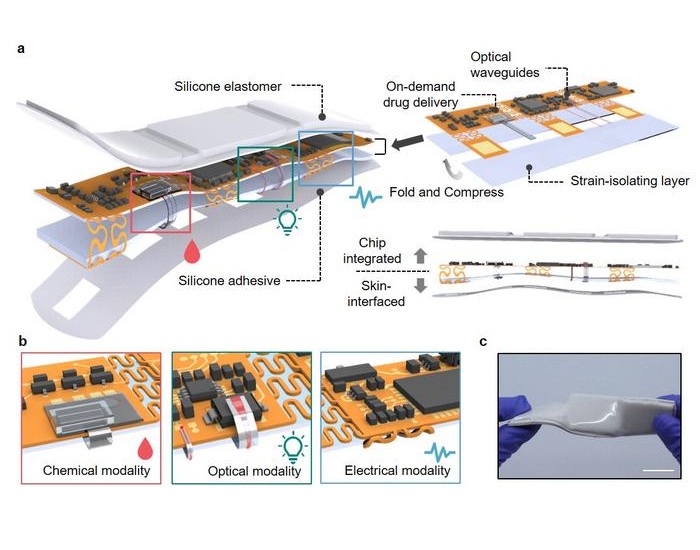
- Wearable Device for Diabetics Could Replace Continuous Glucose Monitoring Systems
- AI Stethoscope Spots Heart Valve Disease Earlier Than GPs
- Bioadhesive Patch Eliminates Cancer Cells That Remain After Brain Tumor Surgery
- Wearable Patch Provides Up-To-The-Minute Readouts of Medication Levels in Body
- New Spray-Mist Device Delivers Antibiotics Directly into Infected Tissue
- Living Implant Could End Daily Insulin Injections
- Intelligent Camera System Continuously Monitors Premature Babies in NICU
- Intranasal Spray to Prevent Illnesses from Respiratory Viruses
- Gut Bacteria from Amphibians and Reptiles Show Complete Tumor Elimination
- High-Dose Inhaled Nitric Oxide Emerges as Promising Antimicrobial Therapy
- AI Risk Prediction Tool Improves Treatment of Cancer Patients after Heart Attack
- Glowing Bacterial Sensors Could Improve Detection of Gut Illness
Channels
Artificial Intelligence
view channelSurgical Techniques
view channelAI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
Lipid-rich plaques inside coronary arteries are strongly associated with heart attacks and other major cardiac events. While optical coherence tomography (OCT) provides detailed images of vessel structure... Read moreNeural Device Regrows Surrounding Skull After Brain Implantation
Placing electronic implants on the brain typically requires removing a portion of the skull, creating challenges for long-term access and safe closure. Current methods often involve temporarily replacing the skull or securing metal plates, which can lead to complications such as skin erosion and additional surgeries.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more