Ventilated COVID-19 Patients Could Benefit from Tracheotomy
|
By HospiMedica International staff writers Posted on 02 Jun 2020 |
Tracheotomy might be reasonable for some patients with COVID-19 who have been ventilated for more than 21 days, according to a new guideline.
Issued by surgeons at the University of Pennsylvania (Penn; Philadelphia, USA) serving on the COVID-19 tracheotomy task force, the guideline highlights specific considerations regarding tracheotomy for patients with COVID-19 that are on ventilatory support. Based on available evidence, they recommend that tracheotomy might be considered in patients with durations of intubation greater than 21 days who are otherwise without significant comorbidities, and who would be expected to have a good prognosis if they survive.
Tracheotomy before 21 days should not be done routinely in these patients solely due to prolonged ventilator dependence, due to the high risk of transmission and poor prognosis of patients requiring intubation and ventilation. Tracheotomy for other indications, such as a known difficult airway, should be considered in COVID-19 patients on a case-by-case basis; when deemed necessary in these patients, an open surgical tracheotomy should be favored over a percutaneous dilational tracheotomy in order to minimize aerosol generation.
Where possible, these tracheotomies should be performed at bedside in a negative pressure room to minimize the risk of transmission during patient transport, and team members in the room should be kept to the minimal critical number, preferably with highly experienced personnel. Airborne and droplet precautions should be followed, and each person in the room should properly don and doff personal protective equipment (PPE). In addition, a multidisciplinary discussion of the patient's goals of care, overall prognosis, and the expected benefits of tracheotomy should be a critical part of the decision-making process. The guideline was published on May 19, 2020, in Annals of Surgery.
“Early tracheostomy must be considered very carefully along with the patient's expected prognosis, as data from some U.S. series suggests that the mortality of intubated patients is still quite high,” said lead author Tiffany Chao, MD. “On the other hand, there are patients who do warrant the procedure for a variety of reasons, which can be done in a way that is safe for the healthcare team, so it should not be avoided in patients with a reasonable indication and prognosis. The optimal timing should continue to be refined as more data is published.”
An estimated 3-17% of patients hospitalized with COVID-19 require invasive mechanical ventilation. While early tracheotomy (within seven days of intubation) is commonly recommended for critically ill ventilated patients without COVID-19, it remains unclear that this would be beneficial for intubated patients with COVID-19, as their mortality is high in any case, and the median duration of intubation of non-survivors appears to be less than a week.
Related Links:
University of Pennsylvania
Issued by surgeons at the University of Pennsylvania (Penn; Philadelphia, USA) serving on the COVID-19 tracheotomy task force, the guideline highlights specific considerations regarding tracheotomy for patients with COVID-19 that are on ventilatory support. Based on available evidence, they recommend that tracheotomy might be considered in patients with durations of intubation greater than 21 days who are otherwise without significant comorbidities, and who would be expected to have a good prognosis if they survive.
Tracheotomy before 21 days should not be done routinely in these patients solely due to prolonged ventilator dependence, due to the high risk of transmission and poor prognosis of patients requiring intubation and ventilation. Tracheotomy for other indications, such as a known difficult airway, should be considered in COVID-19 patients on a case-by-case basis; when deemed necessary in these patients, an open surgical tracheotomy should be favored over a percutaneous dilational tracheotomy in order to minimize aerosol generation.
Where possible, these tracheotomies should be performed at bedside in a negative pressure room to minimize the risk of transmission during patient transport, and team members in the room should be kept to the minimal critical number, preferably with highly experienced personnel. Airborne and droplet precautions should be followed, and each person in the room should properly don and doff personal protective equipment (PPE). In addition, a multidisciplinary discussion of the patient's goals of care, overall prognosis, and the expected benefits of tracheotomy should be a critical part of the decision-making process. The guideline was published on May 19, 2020, in Annals of Surgery.
“Early tracheostomy must be considered very carefully along with the patient's expected prognosis, as data from some U.S. series suggests that the mortality of intubated patients is still quite high,” said lead author Tiffany Chao, MD. “On the other hand, there are patients who do warrant the procedure for a variety of reasons, which can be done in a way that is safe for the healthcare team, so it should not be avoided in patients with a reasonable indication and prognosis. The optimal timing should continue to be refined as more data is published.”
An estimated 3-17% of patients hospitalized with COVID-19 require invasive mechanical ventilation. While early tracheotomy (within seven days of intubation) is commonly recommended for critically ill ventilated patients without COVID-19, it remains unclear that this would be beneficial for intubated patients with COVID-19, as their mortality is high in any case, and the median duration of intubation of non-survivors appears to be less than a week.
Related Links:
University of Pennsylvania
Latest Surgical Techniques News
- Novel Glue Prevents Complications After Breast Cancer Surgery
- Breakthrough Brain Implant Enables Safer and More Precise Drug Delivery
- Bioadhesive Sponge Stops Uncontrolled Internal Bleeding During Surgery
- Revolutionary Nano Bone Material to Accelerate Surgery and Healing
- Superior Orthopedic Implants Combat Infections and Quicken Healing After Surgery
- Laser-Based Technique Eliminates Pancreatic Tumors While Protecting Healthy Tissue
- Surgical Treatment of Severe Carotid Artery Stenosis Benefits Blood-Brain Barrier
- Revolutionary Reusable Duodenoscope Introduces 68-Minute Sterilization
- World's First Transcatheter Smart Implant Monitors and Treats Congestion in Heart Failure
- Hybrid Endoscope Marks Breakthrough in Surgical Visualization
- Robot-Assisted Bronchoscope Diagnoses Tiniest and Hardest to Reach Lung Tumors
- Diamond-Titanium Device Paves Way for Smart Implants that Warn of Disease Progression
- 3D Printable Bio-Active Glass Could Serve as Bone Replacement Material
- Spider-Inspired Magnetic Soft Robots to Perform Minimally Invasive GI Tract Procedures
- Micro Imaging Device Paired with Endoscope Spots Cancers at Earlier Stage
- AI Spine Model Could Reduce Surgical Risks
Channels
Critical Care
view channel
Origami Robots to Deliver Medicine Less Invasively and More Effectively
Delivering medicine to ulcers or other internal sites often requires invasive procedures that can disrupt surrounding tissues and lengthen recovery times. Traditional magnetic actuators used in soft robotics... Read more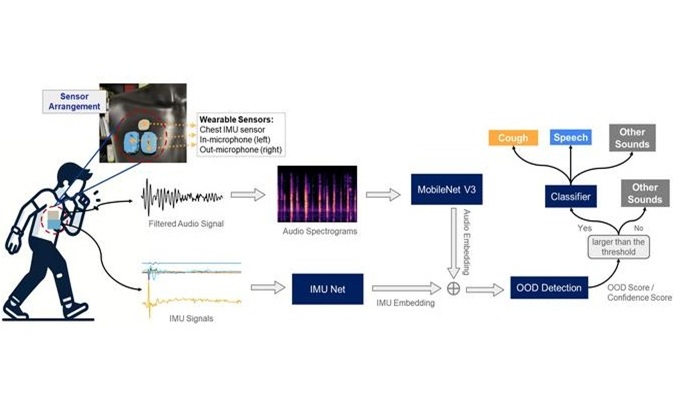
Improved Cough-Detection Technology Aids Health Monitoring
Coughing serves as an important biomarker for tracking a variety of conditions and can help monitor the progress of respiratory diseases or predict when someone’s asthma is being exacerbated.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more














