New AI Algorithm Crunches Massive Amounts of Real-World Data to Find New Uses for Existing Medications
|
By HospiMedica International staff writers Posted on 12 Jan 2021 |

Illustration
Scientists have developed a machine-learning method that crunches massive amounts of data to help determine which existing medications could improve outcomes in diseases for which they are not prescribed.
The aim of this work by researchers at The Ohio State University (Columbus, OH, USA) is to speed up drug repurposing. In order to deem that a drug effective for one disorder will be useful as a treatment for something else, scientists need to conduct time-consuming and expensive randomized clinical trials. Drug repurposing is an attractive pursuit because it could lower the risk associated with safety testing of new medications and dramatically reduce the time it takes to get a drug into the marketplace for clinical use.
Randomized clinical trials are the gold standard for determining a drug’s effectiveness against a disease, although machine learning can account for hundreds – or thousands – of human differences within a large population that could influence how medicine works in the body. These factors, or confounders, ranging from age, sex and race to disease severity and the presence of other illnesses, function as parameters in the deep learning computer algorithm on which the framework is based. That information comes from “real-world evidence,” which is longitudinal observational data about millions of patients captured by electronic medical records or insurance claims and prescription data.
The Ohio State University researchers created a framework that combines enormous patient care-related datasets with high-powered computation to arrive at repurposed drug candidates and the estimated effects of those existing medications on a defined set of outcomes. The research team used insurance claims data on nearly 1.2 million heart-disease patients, which provided information on their assigned treatment, disease outcomes and various values for potential confounders. The deep learning algorithm also has the power to take into account the passage of time in each patient’s experience – for every visit, prescription and diagnostic test. The model input for drugs is based on their active ingredients.
Applying what is called causal inference theory, the researchers categorized, for the purposes of this analysis, the active drug and placebo patient groups that would be found in a clinical trial. The model tracked patients for two years – and compared their disease status at that end point to whether or not they took medications, which drugs they took and when they started the regimen.
Their hypothesis: that the model would identify drugs that could lower the risk for heart failure and stroke in coronary artery disease patients. The model yielded nine drugs considered likely to provide those therapeutic benefits, three of which are currently in use – meaning the analysis identified six candidates for drug repurposing. Among other findings, the analysis suggested that a diabetes medication, metformin, and escitalopram, used to treat depression and anxiety, could lower risk for heart failure and stroke in the model patient population. As it turns out, both of those drugs are currently being tested for their effectiveness against heart disease.
“This work shows how artificial intelligence can be used to ‘test’ a drug on a patient, and speed up hypothesis generation and potentially speed up a clinical trial,” said senior author Ping Zhang, assistant professor of computer science and engineering and biomedical informatics at Ohio State. “But we will never replace the physician – drug decisions will always be made by clinicians.”
Related Links:
The Ohio State University
The aim of this work by researchers at The Ohio State University (Columbus, OH, USA) is to speed up drug repurposing. In order to deem that a drug effective for one disorder will be useful as a treatment for something else, scientists need to conduct time-consuming and expensive randomized clinical trials. Drug repurposing is an attractive pursuit because it could lower the risk associated with safety testing of new medications and dramatically reduce the time it takes to get a drug into the marketplace for clinical use.
Randomized clinical trials are the gold standard for determining a drug’s effectiveness against a disease, although machine learning can account for hundreds – or thousands – of human differences within a large population that could influence how medicine works in the body. These factors, or confounders, ranging from age, sex and race to disease severity and the presence of other illnesses, function as parameters in the deep learning computer algorithm on which the framework is based. That information comes from “real-world evidence,” which is longitudinal observational data about millions of patients captured by electronic medical records or insurance claims and prescription data.
The Ohio State University researchers created a framework that combines enormous patient care-related datasets with high-powered computation to arrive at repurposed drug candidates and the estimated effects of those existing medications on a defined set of outcomes. The research team used insurance claims data on nearly 1.2 million heart-disease patients, which provided information on their assigned treatment, disease outcomes and various values for potential confounders. The deep learning algorithm also has the power to take into account the passage of time in each patient’s experience – for every visit, prescription and diagnostic test. The model input for drugs is based on their active ingredients.
Applying what is called causal inference theory, the researchers categorized, for the purposes of this analysis, the active drug and placebo patient groups that would be found in a clinical trial. The model tracked patients for two years – and compared their disease status at that end point to whether or not they took medications, which drugs they took and when they started the regimen.
Their hypothesis: that the model would identify drugs that could lower the risk for heart failure and stroke in coronary artery disease patients. The model yielded nine drugs considered likely to provide those therapeutic benefits, three of which are currently in use – meaning the analysis identified six candidates for drug repurposing. Among other findings, the analysis suggested that a diabetes medication, metformin, and escitalopram, used to treat depression and anxiety, could lower risk for heart failure and stroke in the model patient population. As it turns out, both of those drugs are currently being tested for their effectiveness against heart disease.
“This work shows how artificial intelligence can be used to ‘test’ a drug on a patient, and speed up hypothesis generation and potentially speed up a clinical trial,” said senior author Ping Zhang, assistant professor of computer science and engineering and biomedical informatics at Ohio State. “But we will never replace the physician – drug decisions will always be made by clinicians.”
Related Links:
The Ohio State University
Latest Business News
- Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
- B. Braun Acquires Digital Microsurgery Company True Digital Surgery
- CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
- Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
- Medtronic Partners with Corsano to Expand Acute Care & Monitoring Portfolio in Europe
- Expanded Collaboration to Transform OR Technology Through AI and Automation
- Becton Dickinson to Spin Out Biosciences and Diagnostic Solutions Business
- Boston Scientific Acquires Medical Device Company SoniVie
- 2026 World Hospital Congress to be Held in Seoul
- Teleflex to Acquire BIOTRONIK’s Vascular Intervention Business
- Philips and Mass General Brigham Collaborate on Improving Patient Care with Live AI-Powered Insights
- Arab Health 2025 Celebrates Landmark 50th Edition
- Boston Scientific Acquires Medical Device Company Intera Oncology
- MEDICA 2024 to Highlight Hot Topics of MedTech Industry
- Start-Ups To Once Again Play Starring Role at MEDICA 2024
- Boston Scientific to Acquire AFib Ablation Company Cortex
Channels
Critical Care
view channel
Pulse Oximeter Index Offers Non-Invasive Guides for Fluid Therapy
In patients with acute circulatory failure, deciding whether to administer intravenous fluids is often a life-or-death decision. Too little fluid can leave organs underperfused, while too much can cause... Read more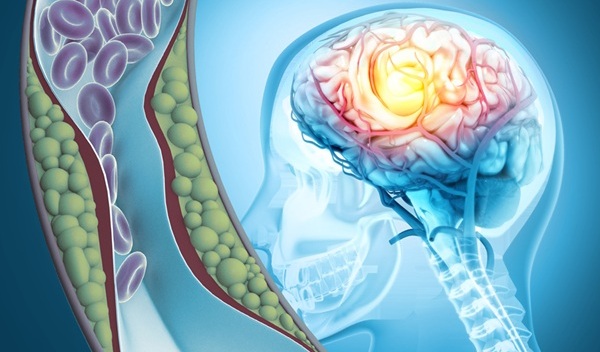
Light-Based Technology to Measure Brain Blood Flow Could Diagnose Stroke and TBI
Monitoring blood flow in the brain is crucial for diagnosing and treating neurological conditions such as stroke, traumatic brain injury (TBI), and vascular dementia. However, current imaging methods like... Read moreSurgical Techniques
view channel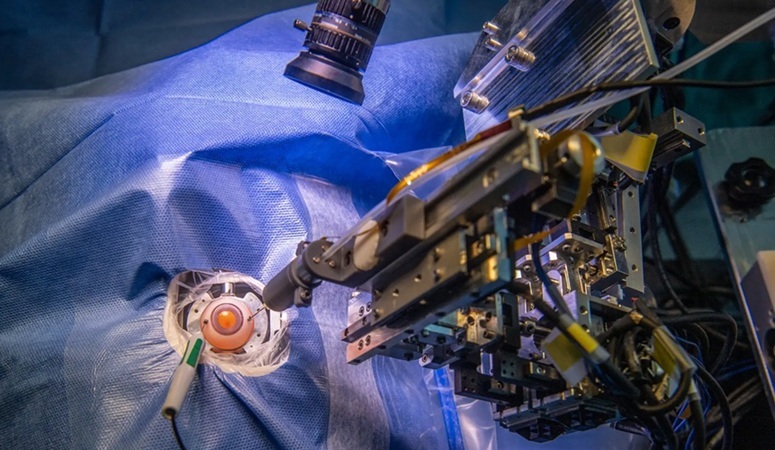
Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting nearly 200 million people, a figure expected to rise to 280 million by 2040. Current treatment involves doctors... Read more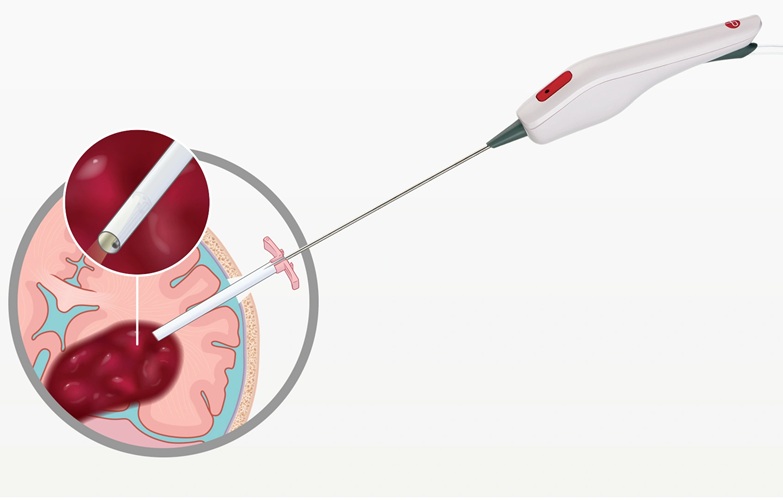
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
















