AI Identifies Severe Aortic Stenosis from Routine ECGs
|
By HospiMedica International staff writers Posted on 02 Sep 2022 |

Aortic stenosis is the most common primary valve lesion requiring surgery or transcatheter intervention in Europe and North America. Prevalence is rapidly increasing due to ageing populations. Guidelines strongly advise early intervention in all symptomatic patients with severe aortic stenosis due to the dismal prognosis. Approximately 50% of untreated patients with aortic stenosis die in the first two years after symptoms appear. Echocardiography is used to assess severity, namely with peak velocity, mean pressure gradient and aortic valve area. However, there is increasing evidence that elevated mortality risk extends beyond current diagnostic definitions and more patients should be considered for aortic valve replacement. Now, a novel artificial intelligence (AI) algorithm uses routine echocardiograms to identify aortic stenosis patients at high risk of death who could benefit from treatment.
Researchers at the University of Notre Dame, Australia (Fremantle, Australia) examined whether an AI algorithm developed from echocardiographic parameters routinely used in clinical practice could identify moderate-to-severe and severe aortic stenosis phenotypes associated with increasing five-year mortality. The proprietary AI-Decision Support Algorithm (AI-DSA) used was trained using data from the National Echo Database of Australia (NEDA), which contains more than 1,000,000 echocardiograms from over 630,000 patients and is linked to mortality information. The algorithm was also trained to ensure all guideline-defined severe aortic stenosis was detected. Training was performed using 70% of the NEDA data, which were randomly selected.
Using the remaining 30% of NEDA data, the researchers compared five-year death rates in patients with the moderate-to-severe and severe aortic stenosis phenotypes with five-year death rates in patients without significant risk of severe aortic stenosis. Out of 179,054 individuals, the AI-DSA identified 2,606 (1.4%) with a moderate-to-severe phenotype and 4,622 (2.5%) with a severe phenotype. Of those with a severe phenotype, 3,566 (77.2%) met guideline criteria for severe aortic stenosis.
The five-year mortality rate was 56.2% in patients with the moderate-to-severe phenotype and 67.9% in those with the severe phenotype. Those without either phenotype (the reference group) had a 22.9% five-year mortality rate. Compared with the reference group, the age- and sex- adjusted odds ratio (OR) for all-cause mortality was 1.82 (95% confidence interval [CI] 1.63–2.02) and 2.80 (95% CI 2.57–3.06) for patients with the moderate-to-severe and severe phenotypes, respectively. Within the severe aortic stenosis phenotype identified by the AI-DSA (4,622; 2.5%), those that met current guidelines (77%) had a five-year mortality of 69.1%. The additional population identified by the AI-DSA with a severe phenotype, but who do not meet current guidelines, had a mortality rate of 64.4%.
“This proprietary AI algorithm picks up patients with a high risk (and all patients within current guidelines) of dying within five years that may be missed by conventional definitions. The findings suggest that the AI algorithm could be used in clinical practice to alert physicians to patients who should undergo further investigations to determine if they qualify for aortic valve replacement,” said principal investigator Professor Geoffrey Strange of the University of Notre Dame, Australia. “Given the rising prevalence of aortic stenosis and its impact on mortality, it is time to revisit the practice of watchful waiting and consider more proactive attempts to identify those at risk. More research is needed to determine if aortic valve replacement improves survival and quality of life in patients identified by the AI-DSA as having a high risk of mortality, but who do not meet current guideline definitions.”
Related Links:
University of Notre Dame, Australia
Latest AI News
Channels
Critical Care
view channel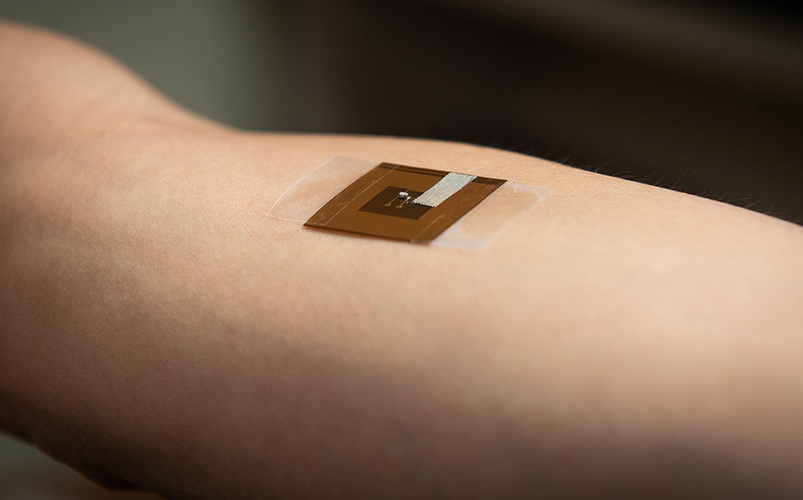
Wearable Patch for Early Skin Cancer Detection to Reduce Unnecessary Biopsies
Skin cancer remains one of the most dangerous and common cancers worldwide, with early detection crucial for improving survival rates. Traditional diagnostic methods—visual inspections, imaging, and biopsies—can... Read more
Pulse Oximeter Index Offers Non-Invasive Guides for Fluid Therapy
In patients with acute circulatory failure, deciding whether to administer intravenous fluids is often a life-or-death decision. Too little fluid can leave organs underperfused, while too much can cause... Read moreSurgical Techniques
view channel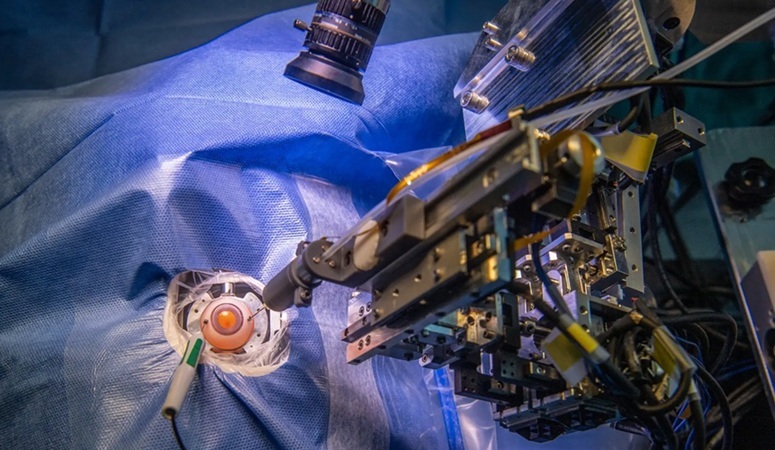
Robotic Assistant Delivers Ultra-Precision Injections with Rapid Setup Times
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting nearly 200 million people, a figure expected to rise to 280 million by 2040. Current treatment involves doctors... Read more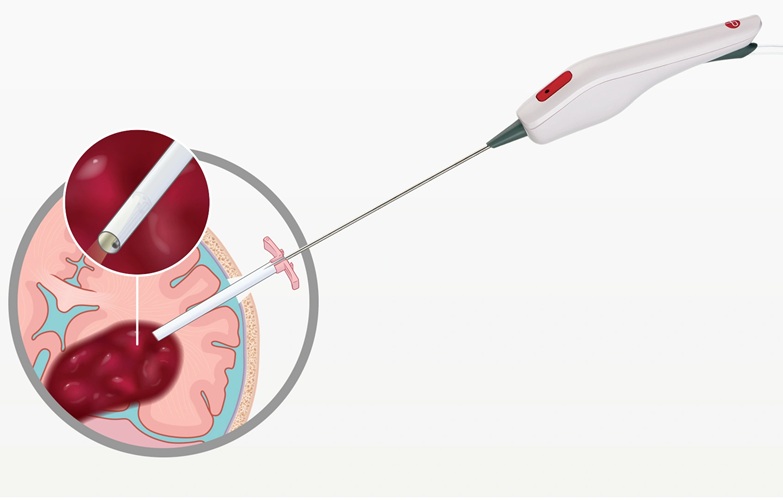
Minimally Invasive Endoscopic Surgery Improves Severe Stroke Outcomes
Intracerebral hemorrhage, a type of stroke caused by bleeding deep within the brain, remains one of the most challenging neurological emergencies to treat. Accounting for about 15% of all strokes, it carries... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
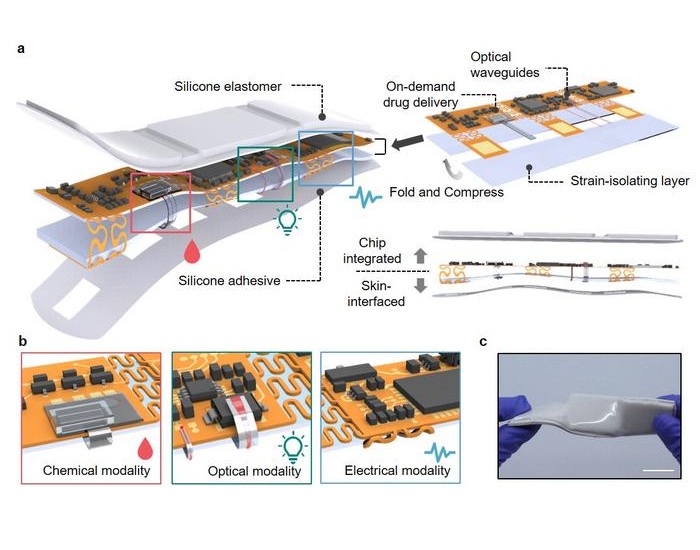
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more