Wearable Device with Stretchable Skin-Like Polymer Sensor Monitors Tumor Size
|
By HospiMedica International staff writers Posted on 19 Sep 2022 |
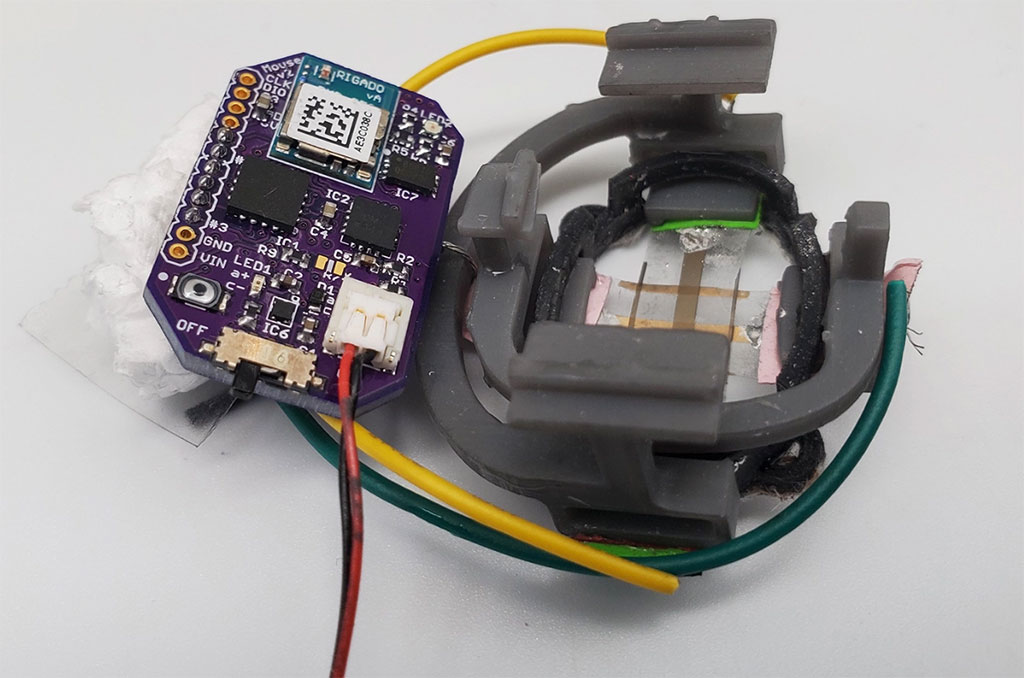
Each year researchers test thousands of potential cancer drugs on mice with subcutaneous tumors. Few make it to human patients, and the process for finding new therapies is slow because technologies for measuring tumor regression from drug treatment take weeks to read out a response. The inherent biological variation of tumors, the shortcomings of existing measuring approaches, and the relatively small sample sizes make drug screenings difficult and labor-intensive. In some cases, the tumors under observation must be measured by hand with calipers. However, the use of metal pincer-like calipers to measure soft tissues is not ideal, and radiological approaches cannot deliver the sort of continuous data needed for real-time assessment. Now, engineers have created a small, autonomous device with a stretchable and flexible sensor that can be adhered to the skin to measure the changing size of tumors below. The non-invasive, battery-operated device is sensitive to one-hundredth of a millimeter (10 micrometers) and can beam results to a smartphone app wirelessly in real time with the press of a button.
The device – dubbed FAST for “Flexible Autonomous Sensor measuring Tumors” – was developed by engineers at Stanford University (Stanford, CA, USA) and represents a wholly new, fast, inexpensive, hands-free, and accurate way to test the efficacy of cancer drugs. On a grander scale, it could lead to promising new directions in cancer treatment. FAST can detect changes in tumor volume on the minute-timescale, while caliper and bioluminescence measurements often require weeks-long observation periods to read out changes in tumor size.
FAST’s sensor is composed of a flexible and stretchable skin-like polymer that includes an embedded layer of gold circuitry. The sensor is connected to a small electronic backpack designed by the Stanford engineers. The device measures the strain on the membrane – how much it stretches or shrinks – and transmits that data to a smartphone. Using the FAST backpack, potential therapies that are linked to tumor size regression can quickly and confidently be excluded as ineffective or fast-tracked for further study. The breakthrough is in FAST’s flexible electronic material. Coated on top of the skin-like polymer is a layer of gold, which, when stretched, develops small cracks that change the electrical conductivity of the material. Stretch the material and number of cracks increases, causing the electronic resistance in the sensor to increase as well. When the material contracts, the cracks come back into contact and conductivity improves.
Based on studies with mice, the researchers say that the new device offers at least three significant advances. First, it provides continuous monitoring, as the sensor is physically connected to the mouse and remains in place over the entire experimental period. Second, the flexible sensor enshrouds the tumor and is therefore able to measure shape changes that are difficult to discern with other methods. Third, FAST is both autonomous and non-invasive. It is connected to the skin – not unlike an adhesive bandage – battery operated, and connected wirelessly. The mouse is free to move unencumbered by the device or wires, and scientists do not need to actively handle the mice following sensor placement. FAST packs are also reusable, cost just USD 60 or so to assemble, and can be attached to the mouse in minutes.
“It is a deceptively simple design,” said Alex Abramson, first author of the study and a recent postdoc in the lab of Zhenan Bao, the K.K. Lee Professor in Chemical Engineering in the Stanford School of Engineering, “but these inherent advantages should be very interesting to the pharmaceutical and oncological communities. FAST could significantly expedite, automate, and lower the cost of the process of screening cancer therapies.”
Related Links:
Stanford University
Latest Critical Care News
- E-Tattoos Harvest Energy and Monitor Health in Real Time
- Focused Ultrasound Tricks Tumors into Marking Themselves for Destruction
- World's Smallest Programmable Robot Opens Up New Possibilities in Medicine
- Remote Ventilate View Platform Enables Real-Time Monitoring of Patient-Ventilator Asynchrony
- Soft “Cyborg” Cardiac Patches Improve Stem Cell Heart Repair
- Soft Wearable System Offers Continuous Wireless Monitoring of Neonatal Health
- AI-Enhanced Wearables Could Transform Type 2 Diabetes and Prediabetes Care
- Breathable Electronic Skin Paves Way for Next-Generation Wearable Devices
- AI Transforming Colon Cancer Diagnosis
- Ventricular Assist Device Offers Long-Term Use in Children Waiting for Donor Heart
- Precision Approach Improves Immunotherapy Effectiveness for ICU Patients with Sepsis
- Soft Robots Could Donate Their Heart to Humans
- Bioadhesive Strategy Prevents Fibrosis Around Device Implants on Peripheral Nerves
- Miniature Non-Invasive Robotic Catheters to Improve Infertility Treatments
- Stick-On Patch Monitors Baby's Movements In Utero
- EEG-Based AI Technology Accurately Diagnoses Alzheimer’s and Dementia
Channels
Surgical Techniques
view channel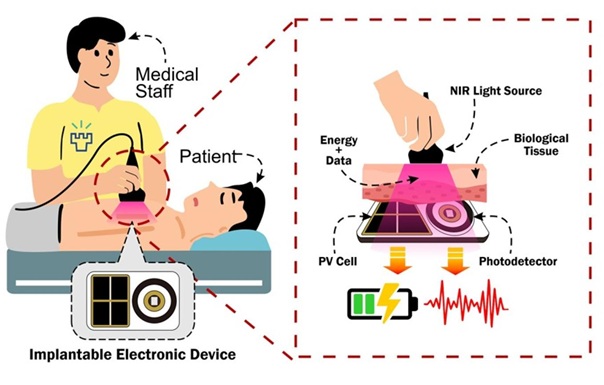
NIR Light Enables Powering and Communicating with Implantable Medical Devices
Implantable medical devices rely on wireless communication and long-lasting power sources to function safely inside the body, yet existing radio-based methods raise concerns around security, interference,... Read more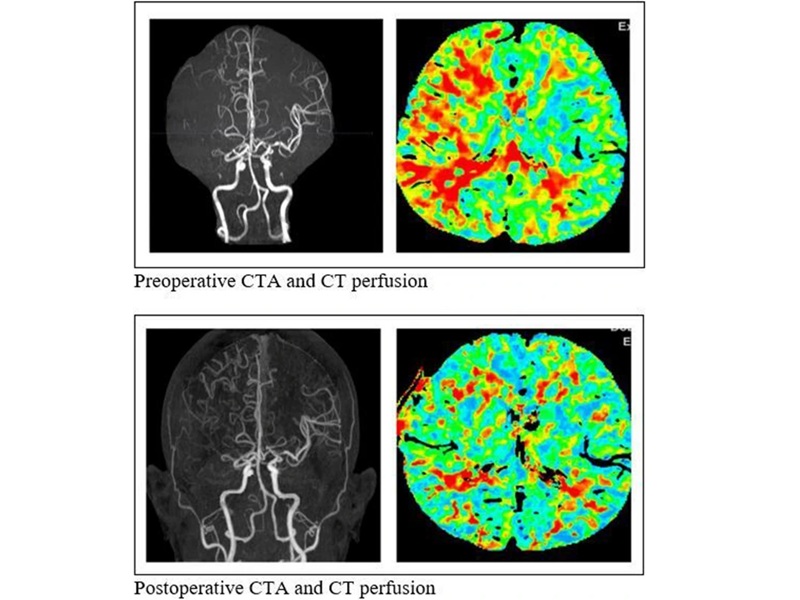
Simple Bypass Protocol Improves Outcomes in Chronic Cerebral Occlusion
Chronic cerebral arterial occlusion and moyamoya disease are major causes of ischemic stroke, particularly in regions where access to advanced diagnostic tools is limited. Assessing cerebral blood flow... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more