New Wireless, Battery-Free Pacemaker Can Be Implanted With Less Invasive Procedure
|
By HospiMedica International staff writers Posted on 28 Oct 2022 |
Atrial fibrillation – a form of irregular heartbeat, or arrhythmia – is estimated to affect approximately 60 million people across the world. Pacemakers are lifesaving devices that regulate the heartbeats of people with chronic heart diseases like atrial fibrillation and other forms of arrhythmia. However, pacemaker implantation is an invasive procedure, and the lifesaving pacing the devices provide can be extremely painful. Additionally, pacemakers can only be used to treat a few specific types of disease. Now, a team of researchers has designed a wireless, battery-free pacemaker that could be implanted with a less invasive procedure than currently possible and would cause patients less pain.
Currently available pacemakers work by implanting one or two leads, or points of contact, into the heart with hooks or screws. If the sensors on these leads detect a dangerous irregularity, they send an electrical shock through the heart to reset the beat. The new device developed by a team of researchers at the University of Arizona (Tucson, AZ, USA), which has not yet been tested in humans, would allow pacemakers to send much more targeted signals using a new digitally manufactured mesh design that encompasses the entire heart. The device uses light and a technique called optogenetics.
Optogenetics modifies cells, usually neurons, sensitive to light, then uses light to affect the behavior of those cells. This technique only targets cardiomyocytes, the cells of the muscle that trigger contraction and make up the beat of the heart. This precision will not only reduce pain for pacemaker patients by bypassing the heart's pain receptors, it will also allow the pacemaker to respond to different kinds of irregularities in more appropriate ways. For example, during atrial fibrillation, the upper and lower chambers of the heart beat asynchronously, and a pacemaker's role is to get the two parts back in line.
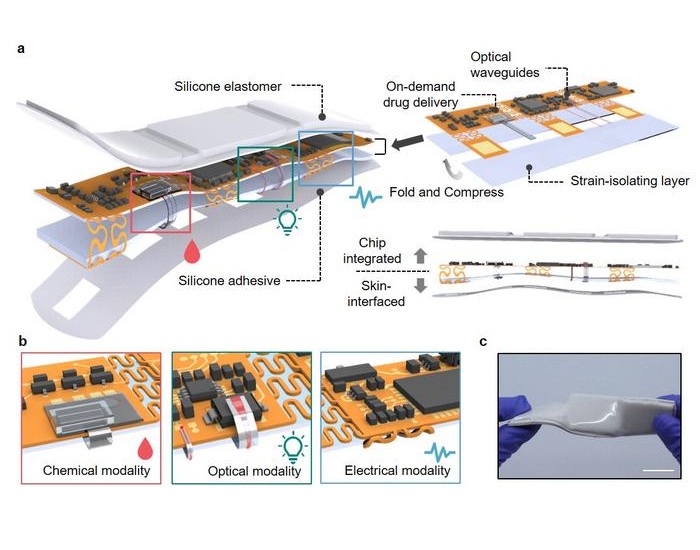
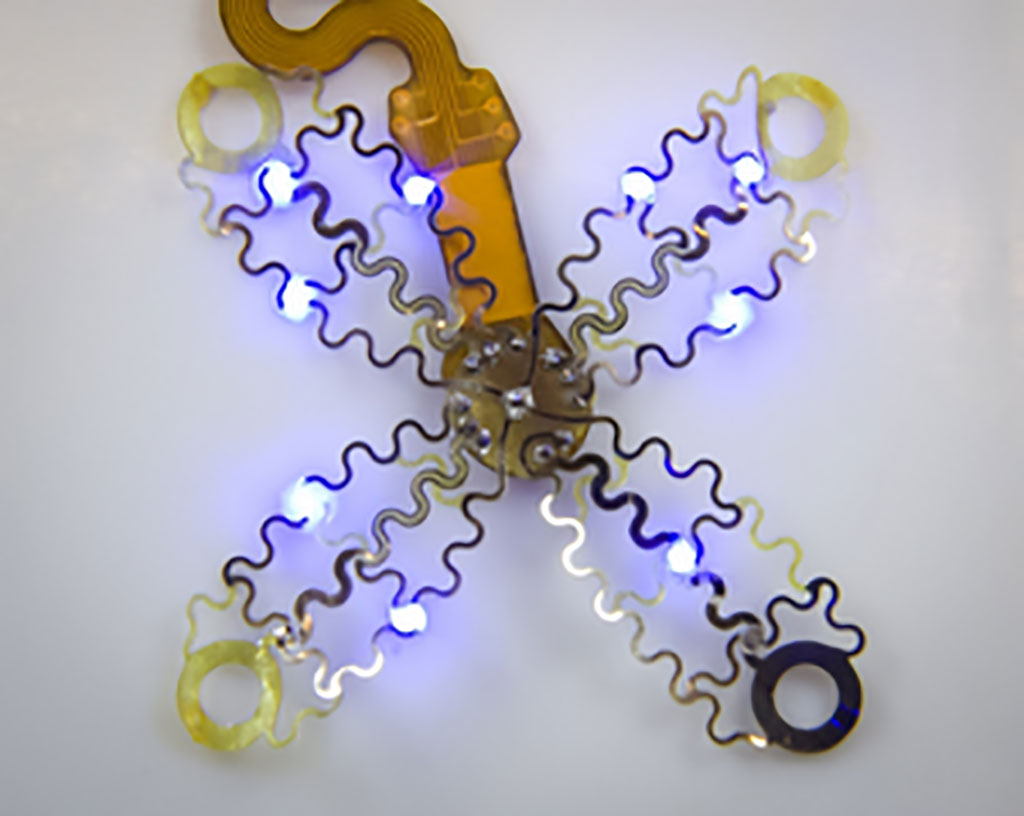
To ensure the light signals can reach many different parts of the heart, the team created a design that involves encompassing the organ, rather than implanting leads that provide limited points of contact. The new pacemaker model consists of four petal-like structures made of thin, flexible film, which contain light sources and a recording electrode. The petals, specially designed to accommodate the way the heart changes shape as it beats, fold up around the sides of the organ to envelop it, like a flower closing up at night.
Because the system uses light to affect the heart, rather than electrical signals, the device can continue recording information even when the pacemaker needs to defibrillate. In current pacemakers, the electrical signal from the defibrillation can interfere with recording capabilities, leaving physicians with an incomplete picture of cardiac episodes. Additionally, the device does not require a battery, which could save pacemaker patients from needing to replace the battery in their device every five to seven years, as is currently the norm.
"All of the cells inside the heart get hit at one time, including the pain receptors, and that's what makes pacing or defibrillation painful. It affects the heart muscle as a whole," said Philipp Gutruf, a biomedical engineering assistant professor and Craig M. Berge Faculty Fellow. "Current pacemakers record basically a simple threshold, and they will tell you, 'This is going into arrhythmia, now shock!' But this device has a computer on board where you can input different algorithms that allow you to pace in a more sophisticated way. It's made for research."
Related Links:
University of Arizona
Latest Surgical Techniques News
- Brain Implant Records Neural Signals and Delivers Precise Medication
- AI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
- Neural Device Regrows Surrounding Skull After Brain Implantation
- Surgical Innovation Cuts Ovarian Cancer Risk by 80%
- New Imaging Combo Offers Hope for High-Risk Heart Patients
- New Classification System Brings Clarity to Brain Tumor Surgery Decisions
- Boengineered Tissue Offers New Hope for Secondary Lymphedema Treatment
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- New AI Approach to Improve Surgical Imaging
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- Ultrasound Device Offers Non-Invasive Treatment for Kidney Stones
- Light-Activated Tissue Adhesive Patch Achieves Rapid and Watertight Neurosurgical Sealing
- Minimally Invasive Coronary Artery Bypass Method Offers Safer Alternative to Open-Heart Surgery
- Injectable Breast ‘Implant’ Offers Alternative to Traditional Surgeries
- AI Detects Stomach Cancer Risk from Upper Endoscopic Images
Channels
Artificial Intelligence
view channelSurgical Techniques
view channel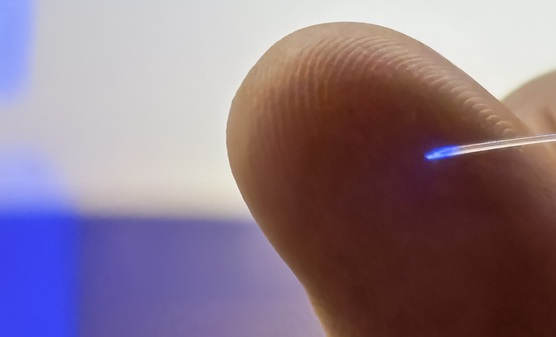
Brain Implant Records Neural Signals and Delivers Precise Medication
Neurological diseases such as epilepsy involve complex interactions across multiple layers of the brain, yet current implants can typically stimulate or record activity from only a single point.... Read moreAI-Based OCT Image Analysis Identifies High-Risk Plaques in Coronary Arteries
Lipid-rich plaques inside coronary arteries are strongly associated with heart attacks and other major cardiac events. While optical coherence tomography (OCT) provides detailed images of vessel structure... Read moreNeural Device Regrows Surrounding Skull After Brain Implantation
Placing electronic implants on the brain typically requires removing a portion of the skull, creating challenges for long-term access and safe closure. Current methods often involve temporarily replacing the skull or securing metal plates, which can lead to complications such as skin erosion and additional surgeries.... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic to Acquire Coronary Artery Medtech Company CathWorks
Medtronic plc (Galway, Ireland) has announced that it will exercise its option to acquire CathWorks (Kfar Saba, Israel), a privately held medical device company, which aims to transform how coronary artery... Read more
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more