Blood- And Urine-Based Biomarker Tests Could Identify Treatment of Acute Kidney Injury
|
By HospiMedica International staff writers Posted on 25 May 2023 |
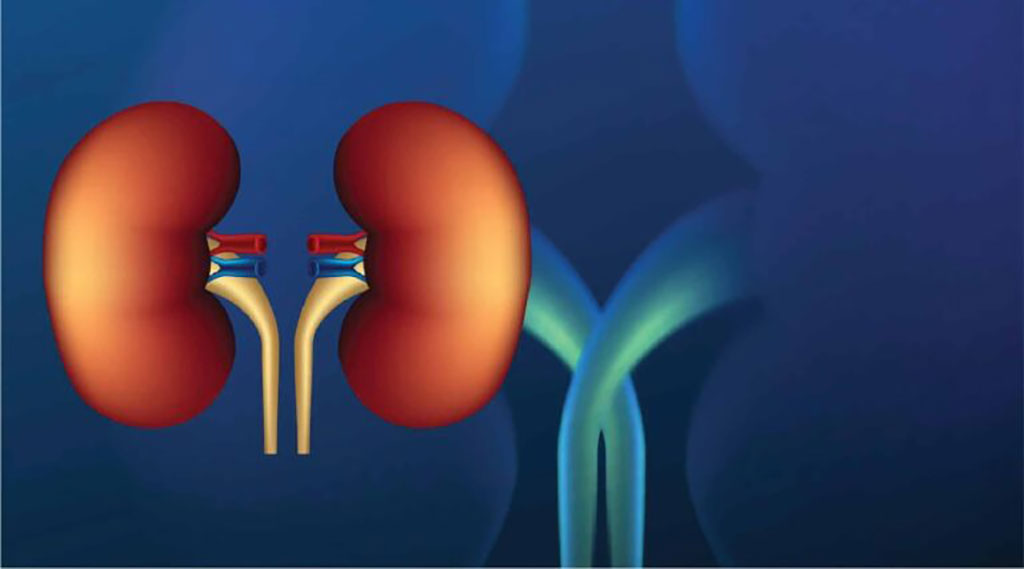
Hospitalized patients who experience an acute kidney injury (AKI) often face unfavorable outcomes post-discharge, with limited effective treatment options. AKI can stem from various causes, such as sepsis, medication, or inadequate blood supply during cardiac bypass. Additionally, different cell types within the kidneys can sustain damage during AKI. Current AKI diagnosis relies on simple kidney function blood tests or measuring changes in urine output. These rudimentary diagnostic methods fail to identify the precise cause of injury or predict which patients are likely to respond better to treatment or recover kidney function. However, that could now change with the advent of new tests for biomarkers to identify the treatment of AKI.
Researchers at UW Medicine (Seattle, WA, USA) led a study involving retrospective analysis of 769 patients with AKI and 769 without the condition, monitoring them for five years post-hospital discharge. They identified two molecularly distinct AKI subgroups, or sub-phenotypes, linked with different risk profiles and long-term outcomes. One group had higher instances of congestive heart failure, while the other exhibited elevated rates of chronic kidney disease and sepsis. The latter group also displayed a 40% increased risk for significant adverse kidney events five years onward, compared to the first group.
Interestingly, factors like sex, diabetes rate, or major surgical procedures as the cause of AKI did not vary across AKI subgroups. This suggests that routinely measured clinical indicators may not forecast the AKI subgroups, necessitating the assessment of blood and urine biomarkers for identification. Based on the findings, the researchers have proposed a strategy to categorize AKI patient subpopulations, aiming to identify therapies tailored to specific patient groups. Similar to how unique biomarkers guide treatments for patient subgroups with cancer or asthma, blood- and urine-based biomarkers could potentially help distinguish subgroups of patients with AKI, resulting in the development of new treatment ideas.
“We’re attempting to better understand the clinical factors and molecular drivers of acute kidney injury so that, in the long run, we can better treat the different ways that people experience this disease process,” said Dr. Jonathan Himmelfarb, a professor of nephrology at the UW School of Medicine and the study’s senior author. “We want to better understand the individual characteristics of people who get acute kidney injury so we can establish common characteristics of subgroup populations of these patients to know whose risk is relatively higher or lower, and work toward treatments specific to their needs.
Related Links:
UW Medicine
Latest Critical Care News
- Magnetically Guided Microrobots to Enable Targeted Drug Delivery

- Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
- Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
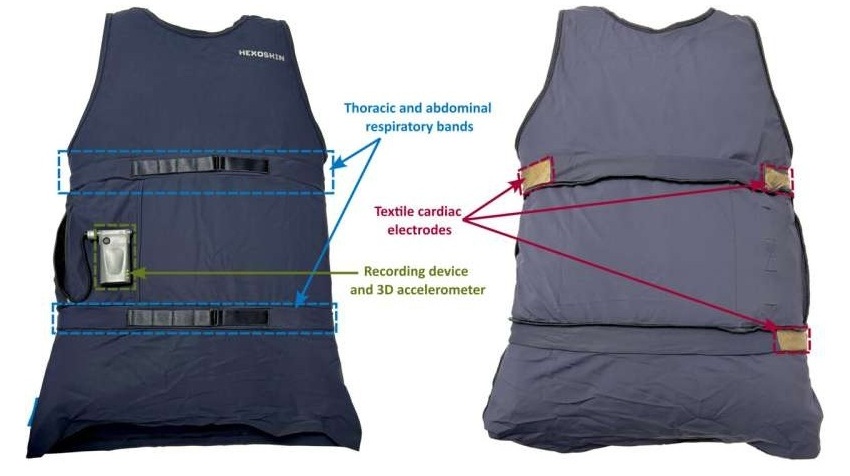
- 'Smart' Shirt Detects Epileptic Seizures in Real Time
- Skin Patch Measures Effectiveness of Flu/COVID Vaccines in 10 Minutes
- Complete Revascularization Reduces Risk of Death from Cardiovascular Causes
- Tiny Fish-Inspired Robots Navigate Through Body to Deliver Targeted Drug Therapy
- Coronary Artery Stenosis Could Protect Patients from Pulmonary Embolism Effects
- Sweat-Powered Sticker Turns Drinking Cup into Health Sensor
- Skin-Mounted 3D Microfluidic Device Analyzes Sweat for Real-Time Health Assessment
- New Therapeutic Brain Implants to Eliminate Need for Surgery
- Stem Cell Patch Gently Heals Damaged Hearts Without Open-Heart Surgery
- Biomaterial Vaccines to Make Implanted Orthopedic Devices Safer
- Deep Learning Model Predicts Sepsis Patients Likely to Benefit from Steroid Treatment
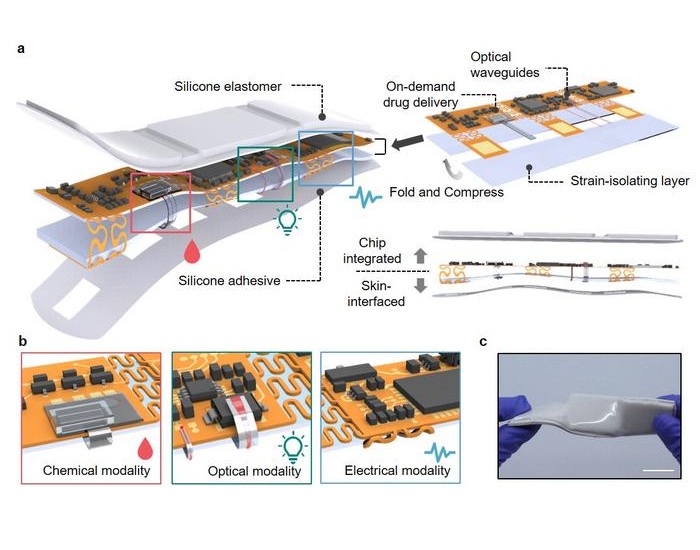
- Programmable Drug-Delivery Patch Promotes Healing and Regrowth After Heart Attack
- Breakthrough Ultrasound Technology Measures Blood Viscosity in Real Time
Channels
Critical Care
view channel
Magnetically Guided Microrobots to Enable Targeted Drug Delivery
Stroke affects 12 million people globally each year, often causing death or lasting disability. Current treatment relies on systemic administration of clot-dissolving drugs, which circulate throughout... Read more
Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
Traumatic brain injury (TBI) continues to leave millions with long-term disabilities every year. After a sudden impact from a fall, collision, or accident, the brain undergoes inflammation, oxidative stress,... Read more
Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
Blood loss during or after surgery can place significant stress on people with heart disease, increasing the risk of dangerous complications. Transfusions are often delayed until hemoglobin levels fall... Read moreSurgical Techniques
view channel
New Study Findings Could Halve Number of Stent Procedures
When a coronary artery becomes acutely blocked during a heart attack, opening it immediately is essential to prevent irreversible damage. However, many patients also have other narrowed vessels that appear... Read more
Breakthrough Surgical Device Redefines Hip Arthroscopy
Hip arthroscopy has surged in popularity, yet surgeons still face major mechanical constraints when navigating deep joint spaces through traditional cannulas. Limited tool mobility and the need for an... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more