Replacement Valve That Grow Inside the Body to Revolutionize Heart Treatment
|
By HospiMedica International staff writers Posted on 01 Feb 2024 |

Heart valve replacement surgery, a life-saving procedure, has been available for over six decades. However, it comes with significant medical limitations, whether the valves used are mechanical or biological. Patients with mechanical heart valves need lifelong medication to prevent blood clotting. Biological valves, in contrast, have a lifespan of only 10 to 15 years. The situation is even more complex for children with congenital heart defects, as their growing bodies necessitate multiple valve replacements before they reach adulthood. Now, recent research suggests that the natural repair mechanisms in humans can be leveraged to build a living heart valve that grows inside the body along with the patient.
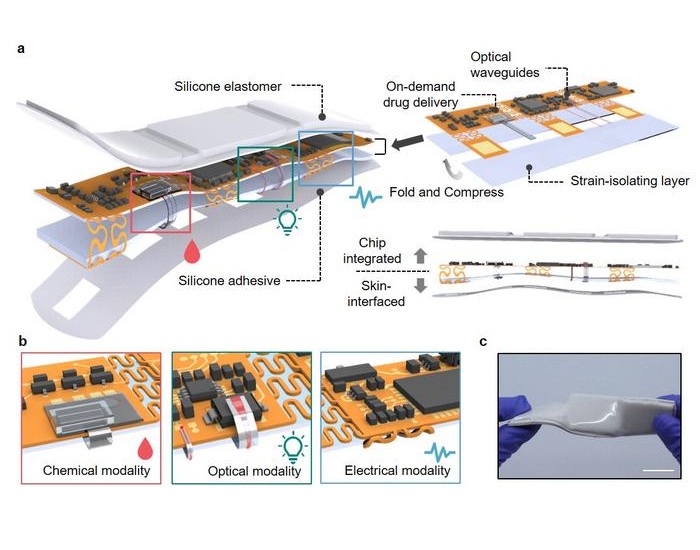
The new approach developed by researchers at Imperial College London (London, UK) involves a procedure that begins with a nanofibrous polymeric valve created from a biodegradable polymer scaffold, unlike the durable plastic that is typically used. Once implanted, this scaffold recruits cells and guides their development, turning the body into a bioreactor for new tissue growth. Over time, the scaffold is naturally replaced by the body's own tissues. At the heart of this innovation is the scaffold material, designed to attract, house, and direct the patient's cells, thereby encouraging tissue growth while preserving valve functionality.
The research team conducted laboratory validation studies and reported the initial results from animal tests. The valves, transplanted into sheep, were observed for up to six months. They functioned effectively throughout this period and demonstrated promising cellular regeneration. Notably, the study highlighted the scaffold's ability to attract blood cells that transform into functional tissues through a process known as endothelial-to-mesenchymal transformation (EndMT). Additionally, nerve and fatty tissue growth within the scaffold was observed, mirroring what one would expect in a normal valve. Concurrently, the polymer scaffold underwent degradation, paving the way for new tissue growth. This degradation was monitored using gel permeability chromatography (GPC) at the Agilent Measurement Suite (AMS) in Imperial’s Molecular Sciences Research Hub in White City, which is equipped with sophisticated analytical tools.
Further research is needed to fully understand the mechanisms behind the polymer's degradation and its correlation with tissue regeneration. The next phase involves extending animal studies to monitor tissue regeneration over longer periods. This data will be vital for obtaining regulatory approval for the first human clinical trials, expected within the next five years. Additionally, refining the manufacturing processes of the valves is necessary. As the project progresses, the team plans to seek commercial partners for later-stage clinical trials. Although currently focused on heart valve replacement, this technology has potential applications in other areas, such as treating vascular conditions, repairing blood vessels damaged by dialysis, and creating cardiac patches for heart repair.
“The aim of the concept we’ve developed is to produce a living valve in the body, which would be able to grow with the patient,” said Dr. Yuan-Tsan Tseng, a biomaterials scientist. “Once you have the scaffold, it becomes a platform technology that you can use to engineer other tissues.”
Related Links:
Imperial College London
Latest Surgical Techniques News
- New Classification System Brings Clarity to Brain Tumor Surgery Decisions
- Boengineered Tissue Offers New Hope for Secondary Lymphedema Treatment
- Dual-Energy Catheter Brings New Flexibility to AFib Ablation
- 3D Bioprinting Pushes Boundaries in Quest for Custom Livers
- New AI Approach to Improve Surgical Imaging
- First-Of-Its-Kind Probe Monitors Fetal Health in Utero During Surgery
- Ultrasound Device Offers Non-Invasive Treatment for Kidney Stones
- Light-Activated Tissue Adhesive Patch Achieves Rapid and Watertight Neurosurgical Sealing
- Minimally Invasive Coronary Artery Bypass Method Offers Safer Alternative to Open-Heart Surgery
- Injectable Breast ‘Implant’ Offers Alternative to Traditional Surgeries
- AI Detects Stomach Cancer Risk from Upper Endoscopic Images
- NIR Light Enables Powering and Communicating with Implantable Medical Devices
- Simple Bypass Protocol Improves Outcomes in Chronic Cerebral Occlusion
- Implantable Absorbable Sensor Detects Life-Threatening Complications After Intestinal Surgery
- New Study Findings Enable Improved Ventilation During Complex Lung Surgery
- 3D-Printed Blood Vessel Scaffolds Could Transform Heart Bypass Surgeries
Channels
Artificial Intelligence
view channelCritical Care
view channel
AI Risk Prediction Tool Improves Treatment of Cancer Patients after Heart Attack
Cancer patients who experience a heart attack face a uniquely dangerous combination of risks, including higher chances of death, bleeding, and repeat cardiac events. Because of this complexity, they have... Read more
Glowing Bacterial Sensors Could Improve Detection of Gut Illness
Diagnosing gastrointestinal diseases often relies on invasive procedures such as endoscopy, which provide only a single snapshot of gut health. These methods make it difficult to track how diseases progress... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Medtronic and Mindray Expand Strategic Partnership to Ambulatory Surgery Centers in the U.S.
Mindray North America and Medtronic have expanded their strategic partnership to bring integrated patient monitoring solutions to ambulatory surgery centers across the United States. The collaboration... Read more
FDA Clearance Expands Robotic Options for Minimally Invasive Heart Surgery
Cardiovascular disease remains the world’s leading cause of death, with nearly 18 million fatalities each year, and more than two million patients undergo open-heart surgery annually, most involving sternotomy.... Read more
WHX in Dubai (formerly Arab Health) to debut specialised Biotech & Life Sciences Zone as sector growth accelerates globally
World Health Expo (WHX) in Dubai, formerly Arab Health, which takes place from 9-12 February 2026 at the Dubai Exhibition Centre (DEC), has officially announced the launch of a new dedicated Biotech &... Read more