New Cellular Immunotherapy Approach Effective In Treating Metastatic Solid Tumors
|
By HospiMedica International staff writers Posted on 12 Jul 2024 |
Chimeric antigen receptor (CAR) T-cell therapy is a form of cellular immunotherapy that has demonstrated effectiveness against certain blood cancers while tumor-infiltrating lymphocyte (TIL) therapy is another form that has shown promise in treating metastatic melanoma. However, finding a cellular therapy that works against other solid cancers has been more challenging. Now, early findings from a small clinical trial suggest that a new cellular immunotherapy approach might be effective for treating metastatic solid tumors.
In the trial, researchers from the National Institutes of Health (NIH, Bethesda, MD, USA) genetically engineered normal white blood cells, or lymphocytes, from patients to produce receptors that target and destroy their specific cancer cells. Their preliminary findings, published on July 11, 2024, in Nature Medicine, are from patients with metastatic colorectal cancer who had undergone multiple prior treatments. This personalized immunotherapy led to tumor shrinkage in several patients and prevented tumor regrowth for up to seven months. The innovation addresses two major hurdles in cellular immunotherapy: producing large quantities of T cells that specifically target cancer cells and boosting the proliferation of these modified T cells after reintroduction into the patient.
For each participant in the study, the team harvested lymphocytes from their tumors. They employed advanced molecular characterization techniques to identify and isolate receptors on those lymphocytes, called T-cell receptors, which recognized specific changes in each patient’s tumor. After genetically sequencing these receptors, the researchers used a retrovirus to insert the receptor genes into normal lymphocytes taken from each patient's blood. These genetically modified lymphocytes were then multiplied into hundreds of millions in the lab and infused back to the patients, where they expressed the tumor-specific T-cell receptors and multiplied further.
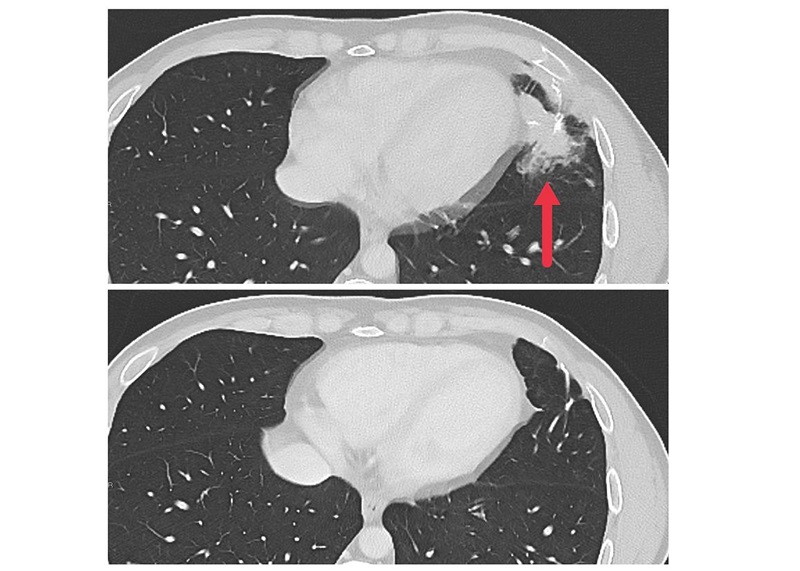
In a subsequent phase 2 trial, seven patients with metastatic colon cancer received this experimental personalized cellular immunotherapy. Before and after the cell therapy, patients were treated with the immunotherapy drugs pembrolizumab and IL-2, respectively. Three of these patients experienced significant reductions in metastatic tumors in the liver, lung, and lymph nodes, with the effects lasting between four to seven months. The median time before disease progression was recorded at 4.6 months. Notably, two of the three responsive patients had T-cell receptors derived from cytotoxic T cells, which are crucial for eliminating diseased cells. The research team is now investigating how to integrate T cell receptors into different subtypes of normal lymphocytes to boost their effectiveness. The ongoing trial is expanding to include patients with various types of solid tumors, exploring broader applications of this therapeutic approach.
“The fact that we can take a growing metastatic solid cancer and get it to regress shows that the new cellular immunotherapy approach has promise,” said Steven A. Rosenberg, M.D., Ph.D., of NCI’s Center for Cancer Research (CCR), who co-led the study. “However, it’s important to understand that these findings are preliminary and that the approach needs to be further refined and tested in more types of solid cancers.”
Related Links:
NIH
Latest Critical Care News
- Magnetically Guided Microrobots to Enable Targeted Drug Delivery

- Smart Nanomaterials Detect and Treat Traumatic Brain Injuries Simultaneously
- Earlier Blood Transfusion Could Reduce Heart Failure and Arrhythmia in Heart Disease Patients
- 'Smart' Shirt Detects Epileptic Seizures in Real Time
- Skin Patch Measures Effectiveness of Flu/COVID Vaccines in 10 Minutes
- Complete Revascularization Reduces Risk of Death from Cardiovascular Causes
- Tiny Fish-Inspired Robots Navigate Through Body to Deliver Targeted Drug Therapy
- Coronary Artery Stenosis Could Protect Patients from Pulmonary Embolism Effects
- Sweat-Powered Sticker Turns Drinking Cup into Health Sensor
- Skin-Mounted 3D Microfluidic Device Analyzes Sweat for Real-Time Health Assessment
- New Therapeutic Brain Implants to Eliminate Need for Surgery
- Stem Cell Patch Gently Heals Damaged Hearts Without Open-Heart Surgery
- Biomaterial Vaccines to Make Implanted Orthopedic Devices Safer
- Deep Learning Model Predicts Sepsis Patients Likely to Benefit from Steroid Treatment
- Programmable Drug-Delivery Patch Promotes Healing and Regrowth After Heart Attack
- Breakthrough Ultrasound Technology Measures Blood Viscosity in Real Time
Channels
Surgical Techniques
view channel
New Study Findings Could Halve Number of Stent Procedures
When a coronary artery becomes acutely blocked during a heart attack, opening it immediately is essential to prevent irreversible damage. However, many patients also have other narrowed vessels that appear... Read more
Breakthrough Surgical Device Redefines Hip Arthroscopy
Hip arthroscopy has surged in popularity, yet surgeons still face major mechanical constraints when navigating deep joint spaces through traditional cannulas. Limited tool mobility and the need for an... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more