Novel Combination of Surgery and Embolization for Subdural Hematoma Reduces Risk of Recurrence
|
By HospiMedica International staff writers Posted on 26 Nov 2024 |
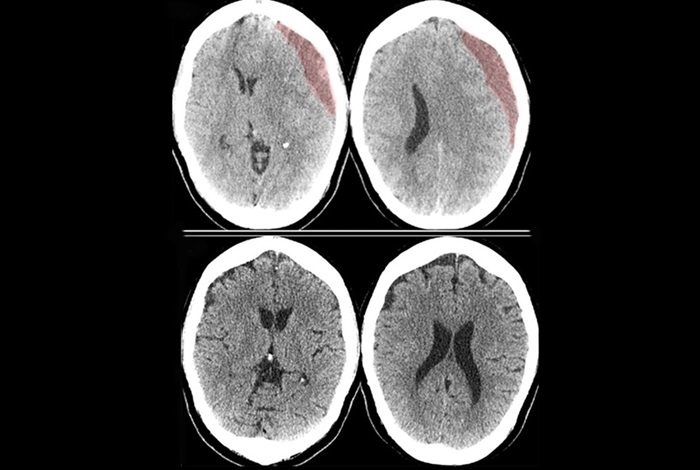
Subdural hematomas, which occur when bleeding happens between the brain and its protective membrane due to trauma, are common in older adults. By 2030, chronic subdural hematomas are expected to become the most prevalent cranial neurosurgical condition globally. Symptoms of a subdural hematoma, such as weakness, numbness, headaches, nausea, confusion, or dizziness, may develop slowly over days or weeks, often following a fall or other head injury. For over a century, doctors have treated symptomatic subdural hematomas through surgery, typically by creating a small hole in the skull or removing a portion of the skull to drain the blood. However, even after the blood is drained, the hematoma can recur about 15% of the time, requiring another surgery and extended hospitalization. This recurrence happens because the hematoma recruits arterial blood vessels that supply it, meaning the condition can return even after surgical drainage. This poses a particular challenge for older patients, who are the primary group affected by chronic subdural hematomas.
Now, researchers at Weill Cornell Medicine (New York, NY, USA) and the University at Buffalo (Getzville, NY, USA) have discovered that a novel combination of surgery and embolization can reduce the risk of recurrence and the need for follow-up surgeries. Embolization is a minimally invasive technique that involves blocking specific blood vessels to halt abnormal bleeding. This discovery comes from the EMBOLISE trial, a multi-center, randomized clinical study that compared the recurrence rates of chronic subdural hematomas in patients treated with surgery and middle meningeal artery (MMA) embolization versus the standard treatment of surgery alone. The study was sponsored by Medtronic (Dublin, Ireland), the company that produces Onyx, the embolic agent used in the treatment group. The MMA embolization procedure involves inserting a small catheter into the middle meningeal artery, which runs through the membranes covering the brain. This catheter delivers an embolic agent that blocks the blood vessels feeding the hematoma. The researchers had previously developed the MMA embolization procedure and published successful preliminary results in 2019.
In their latest research, published in the New England Journal of Medicine, the researchers showed that the combination of MMA embolization and surgery significantly reduced the recurrence of hematomas and the need for additional surgeries. Only about 4% of patients who underwent MMA embolization and surgery experienced recurrence or progression leading to another surgery, compared to more than 11% of patients who had surgery alone. Between December 2020 and August 2023, the study involved 400 adults with chronic subdural hematomas from 39 medical centers. The average age of the patients was 72, and they were randomly assigned to receive either MMA embolization plus surgery (197 in the treatment group) or surgery alone (203 in the control group). Within 90 days of the initial surgery, 4% of the treatment group experienced recurrence or progression requiring another surgery, compared to 11.3% in the control group. Serious adverse events related to MMA embolization occurred in 2% of the patients who underwent the procedure. Researchers are now exploring the potential role of upfront MMA embolization in treating smaller chronic subdural hematomas that may not require surgery. As this may become one of the most common procedures performed by neurosurgeons in the next decade, it holds the potential to lower healthcare costs and improve outcomes for the aging population.
“This trial provides evidence that adding MMA embolization should be a new standard of care for one of the most common neurosurgical conditions we see,” said co-lead author and pioneer of MMA embolization, Dr. Jared Knopman, director of Cerebrovascular Surgery and Interventional Neuroradiology, an associate professor of neurological surgery at Weill Cornell Medicine. “If we embolize these patients early, we may decrease the number who need to be taken to surgery later. In addition to demonstrating the role that the middle meningeal artery plays in the formation and recurrence of subdural hematomas, we have discovered an entirely new facet about the brain that has gone unknown and untreated for decades.”
Latest Surgical Techniques News
- Laparoscopic Surgery Improves Outcomes for Severe Newborn Liver Disease
- Novel Endoscopy Technique Provides Access to Deep Lung Tumors
- New Study Findings Could Halve Number of Stent Procedures
- Breakthrough Surgical Device Redefines Hip Arthroscopy
- Automated System Enables Real-Time "Molecular Pathology" During Cancer Surgery
- Groundbreaking Procedure Combines New Treatments for Liver Tumors
- Ablation Reduces Stroke Risk Associated with Atrial Fibrillation
- Optical Tracking Method Identifies Target Areas in Robot-Assisted Neurosurgery
- General Anesthesia Improves Post-Surgery Outcomes for Acute Stroke Patients
- Drug-Coated Balloons Can Replace Stents Even in Larger Coronary Arteries
- Magnetic Kidney Stone Retrieval Device Outperforms Ureteroscopic Laser Lithotripsy
- Absorbable Skull Device Could Replace Traditional Metal Implants Used After Brain Surgery
- Magic Silicone Liquid Powered Robots Perform MIS in Narrow Cavities
- 'Lab-on-a-Scalpel' Provides Real-Time Surgical Insights for POC Diagnostics in OR
- Biodegradable Brain Implant Prevents Glioblastoma Recurrence
- Tiny 3D Printer Reconstructs Tissues During Vocal Cord Surgery
Channels
Critical Care
view channel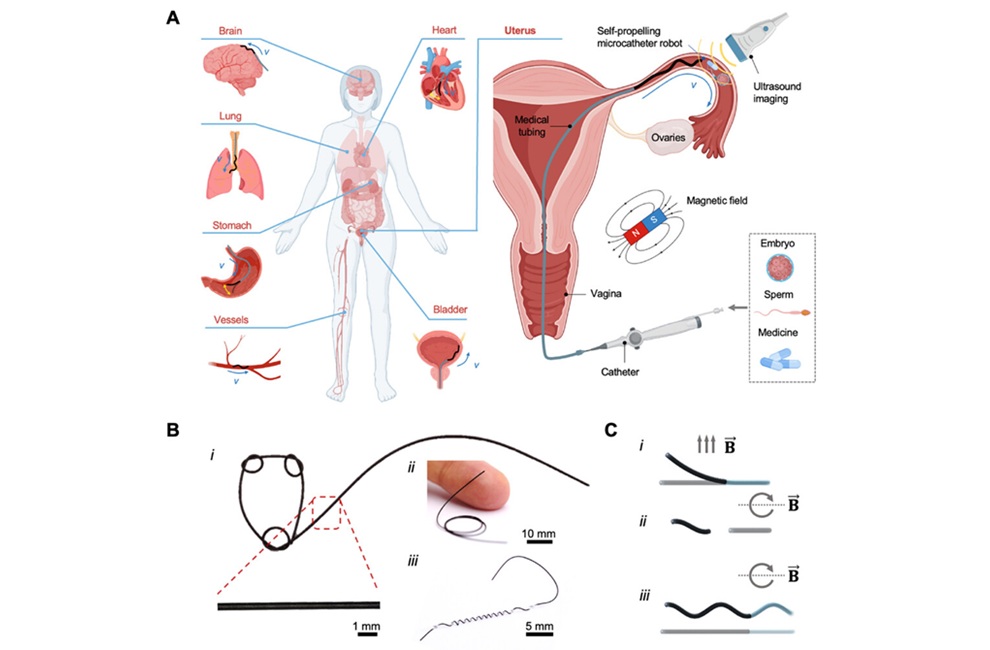
Miniature Non-Invasive Robotic Catheters to Improve Infertility Treatments
Minimally invasive procedures in reproductive and gynaecological medicine are often limited by the difficulty of navigating narrow, delicate anatomical pathways without damaging surrounding tissue.... Read more
Stick-On Patch Monitors Baby's Movements In Utero
Reduced or altered fetal movement is one of the most common reasons expectant parents seek urgent medical care, yet monitoring outside the hospital remains limited. Most pregnant individuals rely on self-counting... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
EMR-Based Tool Predicts Graft Failure After Kidney Transplant
Kidney transplantation offers patients with end-stage kidney disease longer survival and better quality of life than dialysis, yet graft failure remains a major challenge. Although a successful transplant... Read more
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read moreBusiness
view channel
Philips and Masimo Partner to Advance Patient Monitoring Measurement Technologies
Royal Philips (Amsterdam, Netherlands) and Masimo (Irvine, California, USA) have renewed their multi-year strategic collaboration, combining Philips’ expertise in patient monitoring with Masimo’s noninvasive... Read more
B. Braun Acquires Digital Microsurgery Company True Digital Surgery
The high-end microsurgery market in neurosurgery, spine, and ENT is undergoing a significant transformation. Traditional analog microscopes are giving way to digital exoscopes, which provide improved visualization,... Read more
CMEF 2025 to Promote Holistic and High-Quality Development of Medical and Health Industry
The 92nd China International Medical Equipment Fair (CMEF 2025) Autumn Exhibition is scheduled to be held from September 26 to 29 at the China Import and Export Fair Complex (Canton Fair Complex) in Guangzhou.... Read more