Researchers Find Machine Learning Can Improve Patient Care
|
By HospiMedica International staff writers Posted on 07 Sep 2017 |
Image: Researchers developed a machine-learning approach named “ICU Intervene” to ascertain the types of treatments required for various symptoms (Photo courtesy of MIT).
A team of researchers from MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) has developed a machine-learning approach named “ICU Intervene” which uses large amounts of intensive-care-unit (ICU) data, including vitals, labs, notes and demographics, to ascertain the types of treatments required for various symptoms. Using “deep learning,” the system makes real-time predictions by learning from earlier ICU cases to offer suggestions for critical care, along with providing the reasoning for the decisions.
ICU Intervene makes hourly predictions of five different interventions covering various critical care needs, like breathing assistance, improving cardiovascular function, reducing blood pressure, and fluid therapy. The system extracts values from the data representing the vital signs, along with clinical notes and other data points every hour. All this data is represented with values indicating how far away a patient is from the average (for evaluating further treatment).
What is particularly notable is that ICU Intervene can also make future predictions. For instance, the model can predict if a patient will require a ventilator six hours later instead of only 30 minutes or an hour later. The researchers found that the system outperformed the earlier work done in predicting interventions and was particularly good in predicting the requirement for vasopressors. The researchers will focus on improving ICU Intervene in the future to allow for more individualized care and provide more advanced reasoning for decisions, like why the dosage of steroids can be gradually reduced for a patient, or why a procedure such as an endoscopy may be required in the case of another patient.
“The system could potentially be an aid for doctors in the ICU, which is a high-stress, high-demand environment,” according to Harini Suresh, a PhD student and lead author of the paper on ICU Intervene presented in August 2017 at the Machine Learning for Healthcare Conference held in Boston. “The goal is to leverage data from medical records to improve health care and predict actionable interventions.”
Another team of CSAIL researchers has developed “EHR Model Transfer,” an approach to facilitate the application of predictive models on an electronic health record (EHR) system, in spite of being trained on data from a different EHR system. The team used this approach to demonstrate that predictive models for mortality and prolonged length of stay can be trained on one EHR system and used to make predictions in another. The approach can be adopted across different versions of EHR platforms, using natural language processing to identify clinical concepts that are encoded differently across systems and then mapping them to a common set of clinical concepts (such as “blood pressure” and “heart rate”). For instance, in the case of a patient in one EHR platform who could be changing hospitals and would need their data transferred to a different type of platform, the EHR Model Transfer can ensure that the model will still predict aspects of that patient’s ICU visit, such as their chances of a prolonged stay or even of dying in the unit. The researchers plan to evaluate the EHR Model Transfer system on data and EHR systems from other hospitals and care settings in the future.
Related Links:
CSAIL
ICU Intervene makes hourly predictions of five different interventions covering various critical care needs, like breathing assistance, improving cardiovascular function, reducing blood pressure, and fluid therapy. The system extracts values from the data representing the vital signs, along with clinical notes and other data points every hour. All this data is represented with values indicating how far away a patient is from the average (for evaluating further treatment).
What is particularly notable is that ICU Intervene can also make future predictions. For instance, the model can predict if a patient will require a ventilator six hours later instead of only 30 minutes or an hour later. The researchers found that the system outperformed the earlier work done in predicting interventions and was particularly good in predicting the requirement for vasopressors. The researchers will focus on improving ICU Intervene in the future to allow for more individualized care and provide more advanced reasoning for decisions, like why the dosage of steroids can be gradually reduced for a patient, or why a procedure such as an endoscopy may be required in the case of another patient.
“The system could potentially be an aid for doctors in the ICU, which is a high-stress, high-demand environment,” according to Harini Suresh, a PhD student and lead author of the paper on ICU Intervene presented in August 2017 at the Machine Learning for Healthcare Conference held in Boston. “The goal is to leverage data from medical records to improve health care and predict actionable interventions.”
Another team of CSAIL researchers has developed “EHR Model Transfer,” an approach to facilitate the application of predictive models on an electronic health record (EHR) system, in spite of being trained on data from a different EHR system. The team used this approach to demonstrate that predictive models for mortality and prolonged length of stay can be trained on one EHR system and used to make predictions in another. The approach can be adopted across different versions of EHR platforms, using natural language processing to identify clinical concepts that are encoded differently across systems and then mapping them to a common set of clinical concepts (such as “blood pressure” and “heart rate”). For instance, in the case of a patient in one EHR platform who could be changing hospitals and would need their data transferred to a different type of platform, the EHR Model Transfer can ensure that the model will still predict aspects of that patient’s ICU visit, such as their chances of a prolonged stay or even of dying in the unit. The researchers plan to evaluate the EHR Model Transfer system on data and EHR systems from other hospitals and care settings in the future.
Related Links:
CSAIL
Latest AI News
Channels
Critical Care
view channel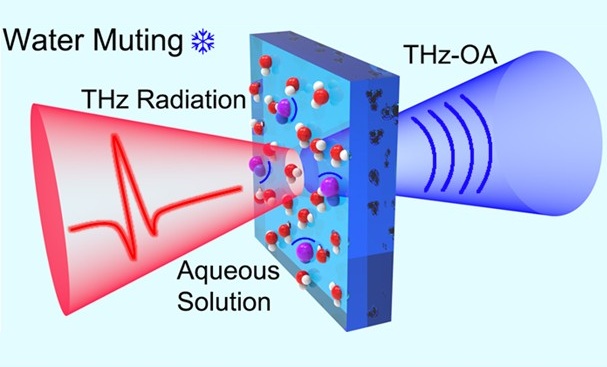
New System Measures Blood Sodium Without Needles
Accurately measuring blood sodium levels is crucial for diagnosing and managing various health conditions, including dehydration, kidney disease, and certain neurological and endocrine disorders.... Read more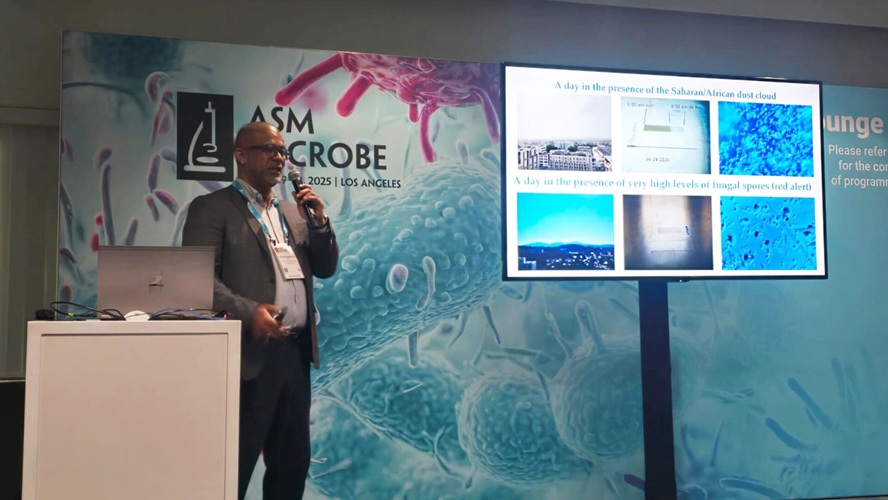
Monitoring Airborne Fungal Spores Could Help Predict COVID-19 & Flu Surges
A new study presented at ASM Microbe 2025 has provided strong evidence that higher levels of fungal spores in the air are closely associated with spikes in influenza and COVID-19 cases. The findings suggest... Read moreSurgical Techniques
view channel
First-Ever Technology Makes Blood Translucent During Surgery
No matter the discipline or scale, bleeding is a regular part of any surgery and can create several challenges. In operating room imaging, seeing through blood in real-time during a surgery has been a... Read more
Tibia Nailing System with Novel Side-Specific Nails to Revolutionize Fracture Surgery
Smith+Nephew (Hull, UK;) has launched its new TRIGEN MAX Tibia Nailing System for stable and unstable fractures of the tibia, including the shaft. It is the only system to now offer trauma surgeons the... Read morePatient Care
view channel
Revolutionary Automatic IV-Line Flushing Device to Enhance Infusion Care
More than 80% of in-hospital patients receive intravenous (IV) therapy. Every dose of IV medicine delivered in a small volume (<250 mL) infusion bag should be followed by subsequent flushing to ensure... Read more
VR Training Tool Combats Contamination of Portable Medical Equipment
Healthcare-associated infections (HAIs) impact one in every 31 patients, cause nearly 100,000 deaths each year, and cost USD 28.4 billion in direct medical expenses. Notably, up to 75% of these infections... Read more
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Bayer and Broad Institute Extend Research Collaboration to Develop New Cardiovascular Therapies
A research collaboration will focus on the joint discovery of novel therapeutic approaches based on findings in human genomics research related to cardiovascular diseases. Bayer (Berlin, Germany) and... Read more