Prolonged ICU Stays Impact Quality of Life
By HospiMedica International staff writers
Posted on 24 Apr 2014
A new study reveals that patients have substantial physical impairments even two years after being discharged from an intensive care unit (ICU).Posted on 24 Apr 2014
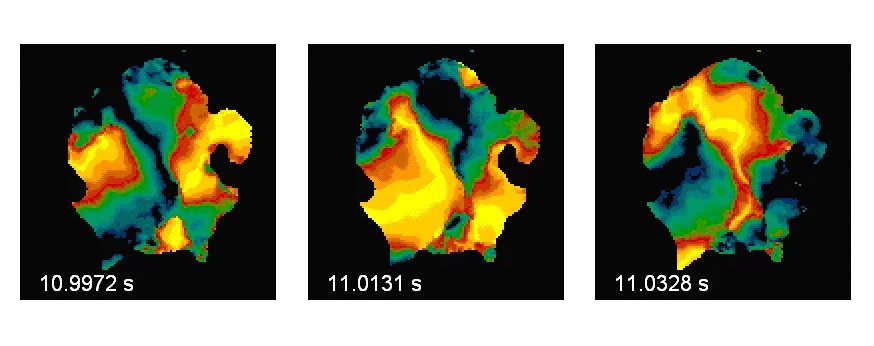
Researchers at Johns Hopkins University (JHU; Baltimore, MD, USA) conducted a prospective observational study involving 222 patients discharged from one of 13 ICUs at four Baltimore (MD, USA) hospitals between October 2004 and October 2007. All patients spent time on a mechanical ventilator as part of their successful treatment for acute lung injury, and underwent evaluation of muscle strength at hospital discharge and also at three, six, 12, and 24 months later.
The results showed that one-third of survivors had muscle weakness at discharge. For every day of bed rest in the ICU, muscle strength was 3%–11% lower over the following months and years. While many saw improvement over time, the weakness was associated with substantial impairments in physical function and quality of life at subsequent follow-up visits. The two variables most associated with muscle weakness were age and the duration of bed rest in the ICU. The study was published in the April 2014 issue of Critical Care Medicine.
“Even a single day of bed rest in the ICU has a lasting impact on weakness, which impacts patients' physical functioning and quality of life,” said lead author Dale Needham, MD, PhD, an associate professor of medicine and of physical medicine and rehabilitation at the JHU School of Medicine. “We previously thought that bed rest and sedation in an ICU were helpful for patients, but we're finding this approach to care is actually harmful to the long-term recovery of many. We need to focus on changing bed rest to improve patients' recovery.”
“The standard of care for really sick patients has been keeping them sedated and in bed,” said coauthor Eddy Fan, MD, PhD. “Many doctors and nurses believe that when there's a breathing tube in place, patients need deep sedation, not rehab. But that is a myth. We need our patients awake and moving.”
Previous research has shown that during the first three days a severely ill patient spends in the ICU, they can expect a 9% decrease in muscle size, due to deep sedation, the use of breathing tubes, and dependency on life-sustaining machinery.
Related Links:
Johns Hopkins University