Smart Insulin Patch Could Replace Painful Injections
By HospiMedica International staff writers
Posted on 23 Jul 2015
A new study describes a novel skin patch that can detect blood sugar levels and secrete doses of insulin whenever needed.Posted on 23 Jul 2015
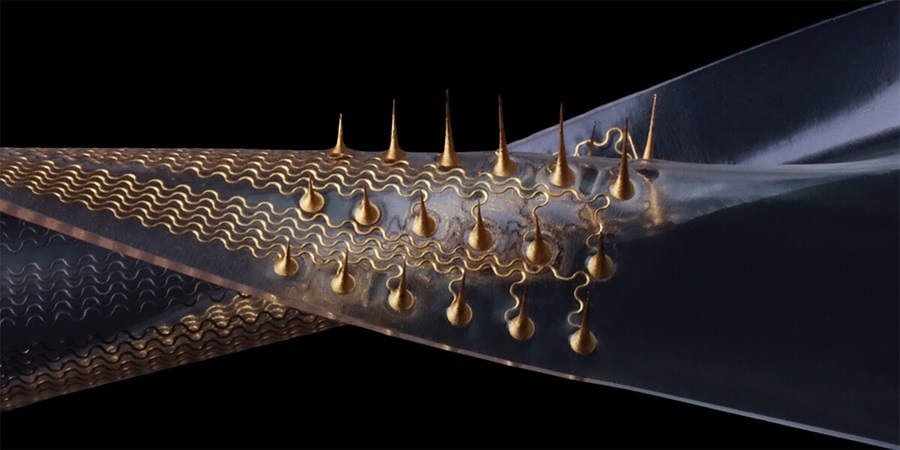
Developed by researchers at North Carolina State University (NCSU; Raleigh, USA) and the University of North Carolina (UNC; Chapel Hill, USA), the insulin patch developed is in essence a glucose-responsive “closed-loop” insulin delivery system that mimics the function of pancreatic beta cells. The patch is based on a microneedle-array containing glucose-responsive vesicles (GRVs) which are loaded with insulin and glucose oxidase (GOx), an enzyme that causes hypoxia when it comes in contact with blood glucose.
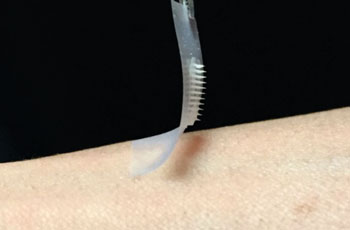
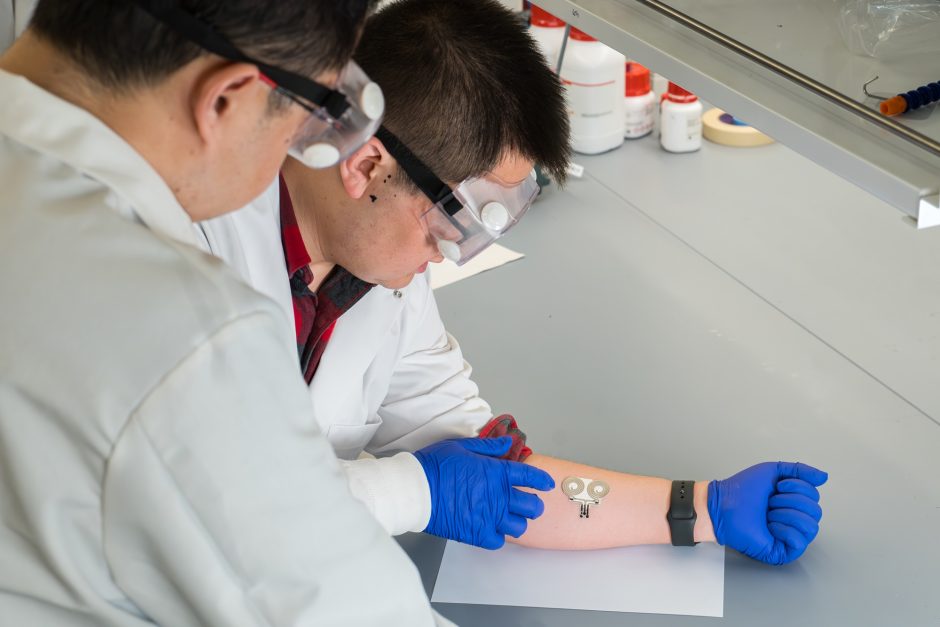
Image: The hyaluronic acid microneedle-array insulin patch (Credit: Courtesy Zhen Gu, PhD/University of North Carolina).
The GRVs, who have an average diameter of 118 nm, are self-assembled from hypoxia-sensitive hyaluronic acid (HS-HA) conjugated with 2-nitroimidazole (NI), a hydrophobic component that undergoes bioreduction under hypoxic conditions. They are incorporated into microneedles made of rigid hyaluronic acid. When the local hypoxic microenvironment caused by the GOx enzymatic oxidation of glucose in the hyperglycemic state causes reduction of HS-HA, a rapid dissociation of the GRVs occurs, with subsequent release of insulin.
The researchers arranged more than one hundred of these microneedles on a thin silicon strip to create the patch. When the patch is placed onto the skin, the microneedles penetrate the surface, tapping into the blood flowing through the capillaries just below. The researchers then tested the patch in a mouse model of chemically induced type 1 diabetes. They found that the microneedle patch effectively regulated the blood glucose within thirty minutes, and stayed that way for several hours. The study was published in the July 7, 2015, issue of Proceedings of the National Academy of Sciences of the United States of America (PNAS).
“We have designed a patch for diabetes that works fast, is easy to use, and is made from nontoxic, biocompatible materials,” said co-senior author Prof. Zhen Gu, PhD, of the joint department of biomedical engineering at NCSU and UNC. “The whole system can be personalized to account for a diabetic’s weight and sensitivity to insulin, so we could make the smart patch even smarter.”
“The hard part of diabetes care is not the insulin shots, or the blood sugar checks, or the diet, but the fact that you have to do them all several times a day every day for the rest of your life,” added co-senior author John Buse, MD, PhD, director of the UNC Diabetes Care Center. “Injecting the wrong amount of medication can lead to significant complications like blindness and limb amputations, or even more disastrous consequences such as diabetic comas and death. If we can get these patches to work in people, it will be a game changer.”
Related Links:
North Carolina State University
University of North Carolina