Earlier Tracheostomies May Benefit COVID-19 Patients
By HospiMedica International staff writers
Posted on 21 Jan 2021
A new study suggests that in SARS-CoV-2 infected patients, a tracheostomy seven to 14 days after initiation of ventilation has better outcomes than waiting another week. Posted on 21 Jan 2021
Researchers at NYU Langone Medical Center (New York, NY, USA) and New York University (NYU, USA) conducted a retrospective review of records of 148 patients with COVID-19 requiring mechanical ventilation between March 1 and May 7, 2020, in order to assess the impact of early tracheostomy in airway management. Outcomes were time from symptom onset to endotracheal intubation; time from endotracheal intubation to tracheostomy; time from tracheostomy to tube downsizing and decannulation; total time on mechanical ventilation; and total length of stay.

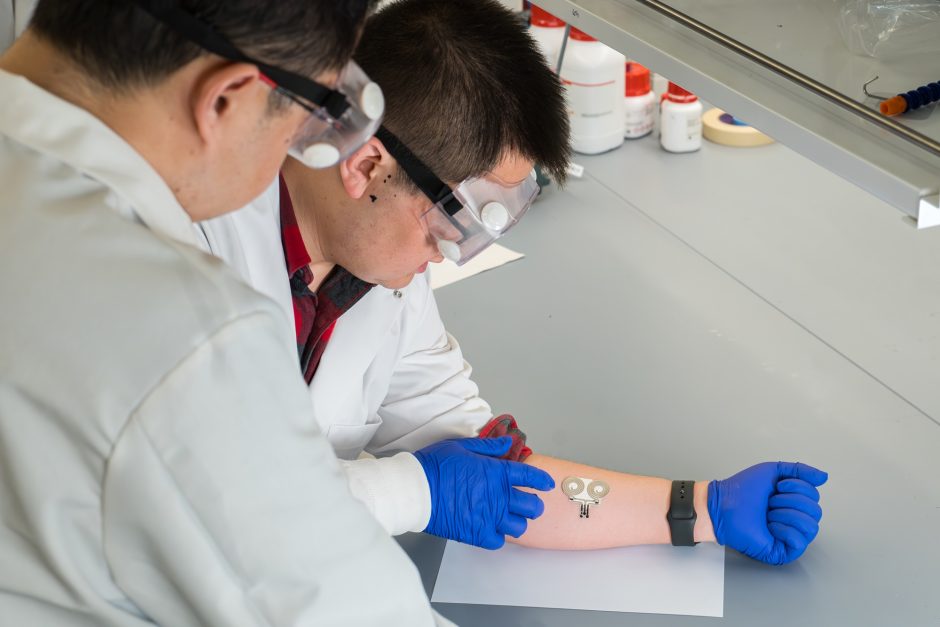
Image: An early tracheostomy in Coronavirus patients can result in better respiratory outcomes (Photo courtesy of Getty Images)
The results showed that for the early tracheostomy group, mean time to tracheostomy was 17.38 days from symptom onset and 5.8 days from intubation. For the late tracheostomy group, the mean time to tracheotomy was 25.69 days from symptom onset and 15.83 days from intubation. The mean time for discontinuing ventilation from intubation was 26.5 days for the early group and 31 days for the late group. In a model with death as the main risk outcome, the late tracheostomy group was 16% less likely to discontinue mechanical ventilation. The study was published on December 17, 2020, in JAMA Otolaryngology-Head & Neck Surgery.
“Early in the pandemic, guidelines based on expert opinion suggested delaying tracheostomy to protect providers. Our concern was that waiting two to three weeks really does predispose patients to airway narrowing and vocal cord paralysis,” said lead author Paul Kwak, MD, of NYU School of Medicine. “Our study demonstrated non-inferiority of early tracheostomy. We saw no increase in infections in surgeons or providers, and this demonstrated the long-term outcomes of these patients indeed were comparable to the late group, with some measures in which the early patients did better.”
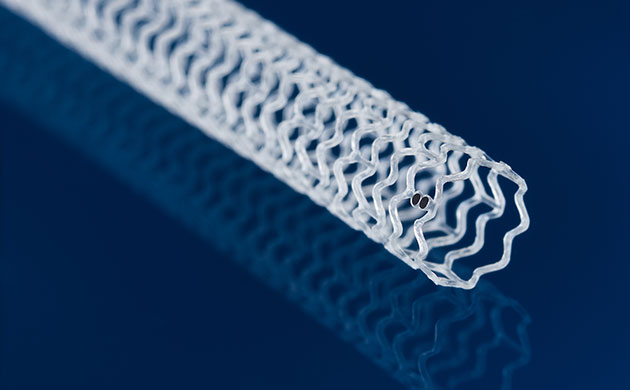
A tracheostomy is a procedure that that creates a stoma on the anterior aspect of the neck, opening a direct airway through the incision in the trachea. A tracheostomy tube is then placed into the opening to provide an air passage when the larynx is blocked or reduced. A tracheostomy is often needed when long-term machine ventilation is required; when no longer needed, it is allowed to heal or is surgically closed.
Related Links:
NYU Langone Medical Center
New York University