Machine Learning Approach Predicts Surgery Duration
By HospiMedica International staff writers
Posted on 01 Aug 2019
A novel artificial intelligence (AI) based statistical model uses large retrospective datasets to improve estimation of surgical procedures duration.Posted on 01 Aug 2019
Researchers at the University of Washington (UW; Seattle, USA) and Perimatics (Bellevue, WA, USA) used a dataset that included 46,986 scheduled surgeries performed by 92 surgeons at UW between January 2014 and December 2017 in order to develop, test, and train machine learning (ML) statistical models that could improve operating room (OR) efficiency by better predicting case-time duration. The models were developed on a training dataset that included 80% of the dataset, and validated on a testing dataset of the remaining 20%.
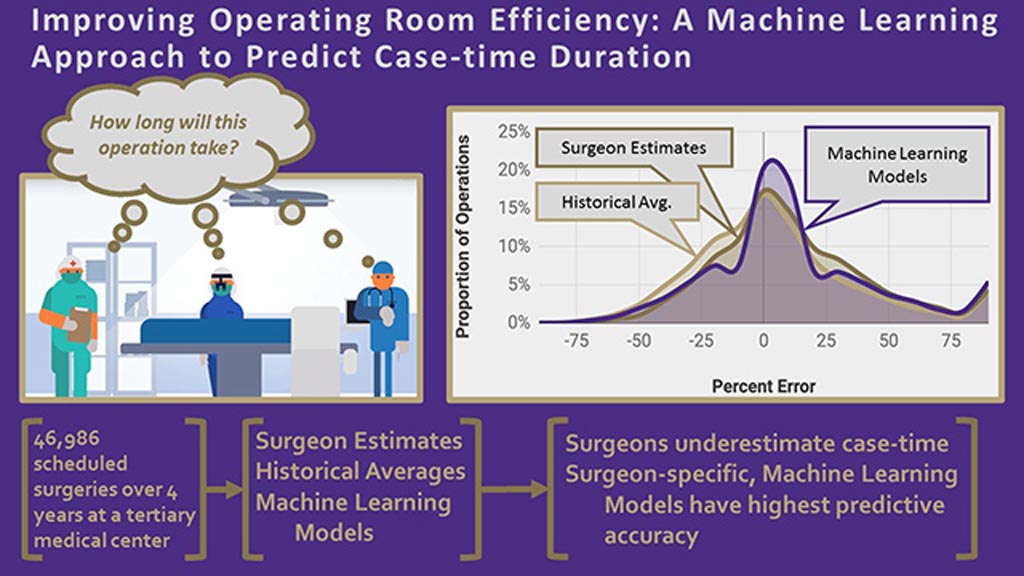
Image: A graphical abstract of the OR AI algorithm (Photo courtesy of UW).
The predictions derived by ML were then compared to average historical procedure times and surgeon estimates, with individual models created for each surgical service and surgeon, respectively. The results showed that the ML algorithm could predict case times within a 10% threshold. Surgeon-specific models were able to improve accuracy from 30% (based on a surgeon's estimate) to 39%, and among the top one-third of surgeons, accuracy improved to more than 50%. The study was published on July 18, 2019, in the Journal of the American College of Surgeons (JACS).
“OR scheduling is a five billion dollar problem. To optimize the OR, you have to answer a fundamental question: How long does each surgery take? Underutilization means fewer patients get surgical care and the hospital has excess capacity. Overutilization results in cancelled operations and overtime expenses,” said study co-lead author Rajeev Saxena, MD, of the UW School of Medicine. “You can change an entire organizational culture by taking a data-forward approach and engaging key stakeholders.”
Many variables need to be considered when attempting to optimize surgical scheduling, including case duration, patient waiting time for surgery, and the number of blocks of OR time given to each surgeon or surgical service, as determined by OR committees. A utilization threshold of 75% is appropriate for most ORs, but if a hospital can strengthen OR utilization, it can grow revenue by increasing total case volume.
Related Links:
University of Washington
Perimatics