New Blood Test Predicts Sepsis in Burn Patients
By HospiMedica International staff writers
Posted on 20 Jul 2016
A new study suggests that measuring three biomarkers of neutrophil function could help determine which burn victims are likely to develop sepsis during their treatment.Posted on 20 Jul 2016
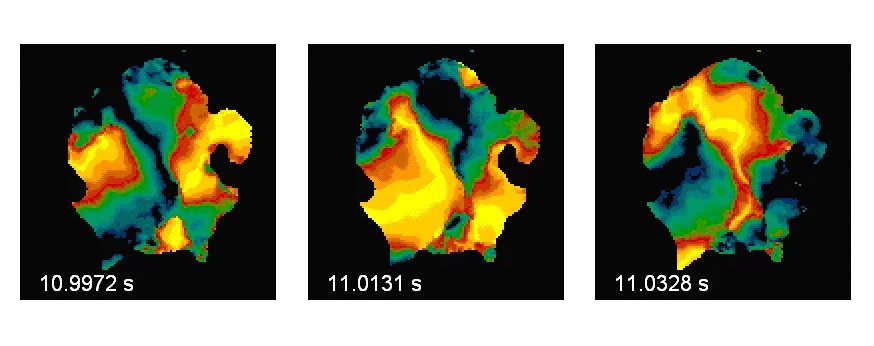
Researchers at the University of Birmingham (UB; United Kingdom) and Queen Elizabeth Hospital Birmingham (QEHB; United Kingdom), conducted a study in 62 patients admitted to the QEHB Burns Centre with 39% burns (on average), who were recruited within 24 hours of their injury. The researchers measured peripheral blood neutrophil function and biomarkers of neutrophil phagocytosis, oxidative burst capacity, and neutrophil extracellular trap (NET). The patients where then monitored in the weeks following for development of sepsis.

Image: Researchers have created a new test that will allow clinicians to predict which burn victims will develop sepsis during their treatment (Photo courtesy of the University of Birmingham).
In addition, three potential biomarkers of sepsis were tracked - immature granulocyte (IG) count, plasma citrullinated histone H3 (Cit H3), and plasma cell-free DNA (cfDNA). The researchers found that neutrophil function was reduced in a greater degree in patients who developed sepsis, which was also characterized by elevated IG, Plasma cfDNA, and Cit-H3 during septic episodes. The researchers concluded that measurement of the three markers at the first post-injury day gave good discriminatory power for the identifying potentially septic patients. The study was published on May 26, 2016, in Annals of Surgery.
“The researchers have shown that burn patients who may suffer life threatening systemic infections, which occur in 30% of major burns at around day six following their injury, could be identified with a 98.6% certainty,” said study co-author Mr Naiem Moiemen, burns and plastics consultant at QEHB. “Burn patients who suffer systemic infection have a high probability of non-surviving their injury. This discovery will enable the clinicians to stratify the care of these patients and improve their outcomes.”
“Major burn injuries result in a systemic inflammatory response syndrome (SIRS) and reduced immune function, which increases the risk of patients developing sepsis or infections in hospitals. Administration of antibiotics within three hours after sepsis recognition is recommended, but only when positive blood cultures are present,” said senior author Professor Janet Lord, PhD, director of the UB institute of inflammation and ageing. “However, the majority of clinical studies report negative cultures in as many as 40% of severe sepsis patients, so many cases will be missed. As such, the identification of novel, accurate biomarkers is crucial.”
Neutrophils are the most abundant (40-75 %) type of white blood cells (WBCs) in mammals, and form an essential part of the innate immune system. Normally found in the bloodstream, they are short-lived and highly motile, recruited to the site of an injury by chemotaxis within minutes following trauma. They are also the predominant cells in pus, accounting for its whitish/yellowish appearance.
Related Links:
University of Birmingham
Queen Elizabeth Hospital Birmingham