Meniscal Knee Surgery May Lead to Arthritis and Cartilage Loss
By HospiMedica International staff writers
Posted on 29 Dec 2014
A widely used surgical procedure to repair meniscal tears may increase the risk of osteoarthritis and cartilage loss in some patients, according to new research. In the study, 100% of knees that had undergone surgery went on to develop arthritis, compared to 59% of those that had meniscal damage but did not have surgery.Posted on 29 Dec 2014
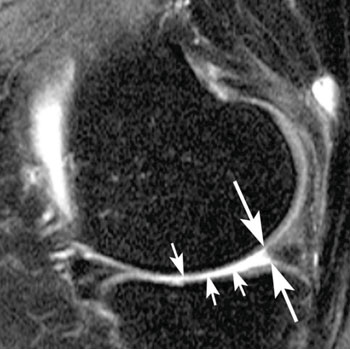
The study’s findings were presented December 3, 2014, at the annual meeting of the Radiological Society of North America (RSNA), held in Chicago (IL, USA). The findings show that the decision for surgery requires cautious consideration to avoid faster disease onset, researchers reported. The new study centered on the meniscus, a wedge-shaped portion of the cartilage in the knee that acts as a shock absorber between the femur and tibia. The two menisci in each knee also play a significant role in joint stability. Meniscal tears are among the most common knee injuries, and surgery is frequently performed to lessen pain.
“Meniscal surgery is one of the most common orthopedic procedures performed to alleviate pain and improve joint function,” said Frank W. Roemer, MD, from the Boston University School of Medicine (Boston, MA, USA) and the University of Erlangen-Nuremberg (Erlangen, Germany). “However, increasing evidence is emerging that suggests meniscal surgery may be detrimental to the knee joint.”
Dr. Roemer and colleagues examined data from the Osteoarthritis Initiative, a large, ongoing observational study of knee osteoarthritis incidence and progression. Patients in the study were on average 60.2 years old and predominantly overweight, with a mean body mass index (BMI) of 28.3. Approximately two-thirds of the patients were women.
The researchers assessed magnetic resonance imaging (MRI) scans of 355 knees that developed osteoarthritis during a five-year period, and a control group that was matched for age, gender, arthritic severity in both knees and BMI. Out of all the knees, 31 underwent meniscal surgery during the year prior to the arthritis diagnosis, and 280 knees had signs of meniscal damage on MRI but did not have surgery. Additionally, part of the study included control cases with no meniscal damage. The researchers assessed the risk of developing arthritis and cartilage loss during the following year for the different groups.
“We found that patients without knee osteoarthritis who underwent meniscal surgery had a highly increased risk for developing osteoarthritis and cartilage loss in the following year compared to those that did not have surgery, regardless of presence or absence of a meniscal tear in the year before,” Dr. Roemer said.
All 31 of the knees that underwent meniscal surgery during the prior year developed osteoarthritis, compared with 165 (59%) of the knees with meniscal damage that did not have surgery. Furthermore, cartilage loss was much more common among knees that had undergone surgery: 80.8% of knees with surgery showed cartilage loss, compared with 39.5% of knees with meniscal damage and no surgery.
An alternative to surgery is conservative management. In conservative management, physical therapy is recommended to help maintain and restore muscle strength and range of motion. Symptoms are typically treated with ice and nonsteroidal anti-inflammatory drugs.
“The indications for meniscal surgery might need to be discussed more carefully in order to avoid accelerated knee joint degeneration,” Dr. Roemer concluded.
Related Links:
Boston University School of Medicine
University of Erlangen-Nuremberg