Targeted Optical Fluorescence Lights Up Lung Cancer
By HospiMedica International staff writers
Posted on 20 Aug 2015
New intraoperative imaging technology allows for visualization of tumor margins and accurate selection of involved lymph nodes, according to a new study. Posted on 20 Aug 2015
Researchers at the University of Pennsylvania (Philadelphia, PA, USA) designed a study to examine the feasibility of using a targeted molecular contrast agent that can bind to lung cancers, which could then be identified using real-time optical imaging during excision surgery. To do so, 50 patients with a biopsy-proven lung adenocarcinoma were enrolled. Before surgery, the patients were administered with 0.1 mg/kg of folate-fluorescein isothiocyanate (FFI), a molecular contrast agent delivered by intravenous (IV) infusion.
FFI binds to folate receptor alpha (FRalpha), a cell surface protein expressed on the exposed surface of adenocarcinoma at a rate of 103–104 receptors per cell; four tumors were not fluorescent, since they did not express FRalpha. During surgery, the tumors were imaged in situ and ex-vivo, after the lung parenchyma was dissected to directly expose the tumor to the imaging system. This was necessary since molecular imaging could identify only seven of the 50 adenocarcinomas in situ, since tumors one centimeter or more below the pleural surface were not detectable until they were removed.
After examining all the excised tissues, the researchers found that the lung adenocarcinomas ranged from 0.3–7.5 cm in diameter, and 92% of them were fluorescent. No false uptake occurred, and in two cases, intraoperative imaging revealed tumor metastases not recognized preoperatively. The researchers found that the most important predictor of success was the distance of the cancerous nodule from the pleural surface. The study was published in the July 2015 issue of the Journal of Thoracic and Cardiovascular Surgery.
“This technology will permit precise visualization of tumor margins, localization of small malignant ground glass opacities, and accurate selection of lymph nodes with metastatic cancer cells. With miniaturization of imaging devices, this method will be particularly useful in minimally invasive surgery,” concluded senior author Sunil Singhal, MD, of the department of surgery, and colleagues. “In the future, with improved devices and molecular contrast agents, this approach may reduce the local recurrence rate and improve intraoperative identification of metastatic cancer cells.”
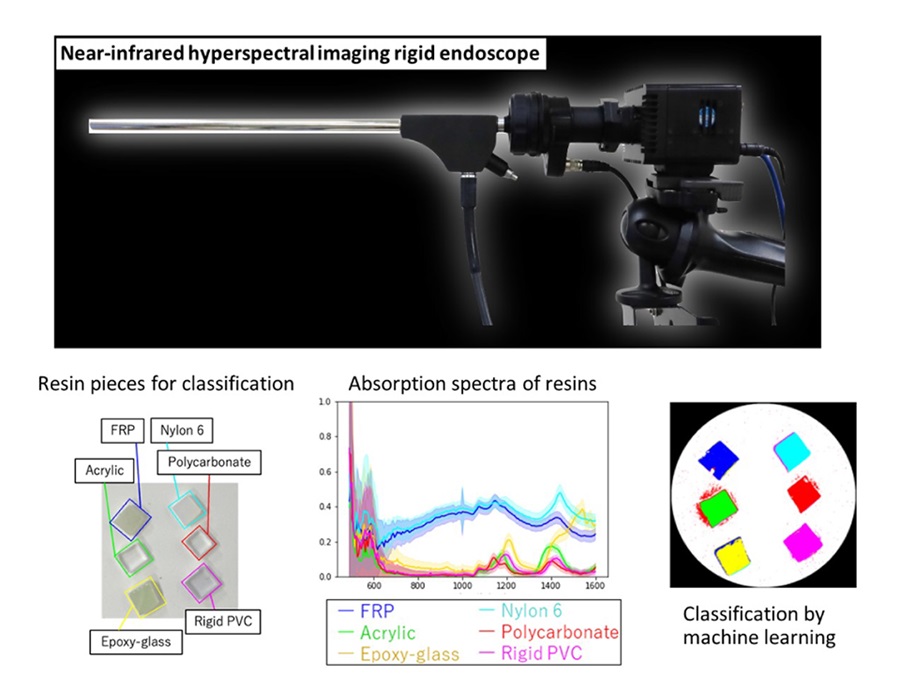
The researchers also suggested two possible refinements to overcome the 1-cm limitation. The first was using spectroscopic tools to analyze scatter from the fluorescent moiety. Adopting this approach could allow deeper penetration, as much as several centimeters, into the solid organ. The second option was to redesign the tracer for near-infrared (NIR) capabilities. The NIR tracer could then provide greater tissue penetration and reduced autofluorescence, allowing the detection of nodules buried deeper beneath the overlying healthy parenchyma.
Related Links:
University of Pennsylvania