Understanding Post-Operative Loss of Vision
|
By HospiMedica International staff writers Posted on 28 Oct 2008 |
A new review of the studies, findings, and current literature regarding loss of vision after non-ocular surgery provides recommendations for surgical teams in preventing this tragic complication.
The review, written by researchers the University of Illinois (Chicago, IL, USA), covers the results of two large retrospective studies, which show that post-operative visual loss (POVL) can be as high as 4.5% in cardiac surgery and 0.2% in spine surgery. There are several causes of POVL after non-ocular surgery, including ischemic optic neuropathy, central retinal artery or vein occlusion, and cortical blindness. In fact, any interruption of blood supply to the eyes during surgery--whether caused by pressure to the eye itself or to the blood supply--or an interruption to the patient's blood flow autoregulation system can lead to POVL. One study showed that there was a higher increase of intraocular pressure (IOP) in patients whose heads were supported by pillows versus patients whose heads were supported by pins in the prone position. Another study demonstrated that as time spent in the prone position increased, IOP continued to increase as well. Some authors have suggested that IOP may increase as a result of large amounts of intravenous (IV) fluids given during surgery.
A variety of factors have been identified that contribute to the various causes of POVL, some intrinsic to the patient that can be thought of as predisposing factors, while others are related more directly to surgery and anesthesia. One study concluded that consideration should be given to establishing a minimum systolic blood pressure for each patient as well as staging long procedures and protecting eye position during surgery. Other recommendations include careful preoperative history to identify any preexisting patient risk factors that predispose to POVL; considered use of deliberate hypotension in patients at risk; avoidance of compression of the eyes, abdomen, or chest in patients placed prone; and correction of anemia and/or hypotension as early as is feasible upon identification of these risk factors. The study was published in the October 2008 issue of Neuro-Ophthalmology.
"Determining the actual overall incidence of POVL is difficult since it is not known what percentage of cases is reported,” said lead author, Molly Gilbert, M.D., an assistant professor of ophthalmology at the University of Illinois Eye and Ear Infirmary. "A wide variety of surgical interventions have been associated with POVL, including cardiopulmonary bypass, lumbar spine surgery, neck dissection, abdominal procedures, hip surgery, cholecystectomy, parathyroidectomy, prostate surgery, pleurodesis, and rotator cuff surgery.”
Related Links:
University of Illinois
The review, written by researchers the University of Illinois (Chicago, IL, USA), covers the results of two large retrospective studies, which show that post-operative visual loss (POVL) can be as high as 4.5% in cardiac surgery and 0.2% in spine surgery. There are several causes of POVL after non-ocular surgery, including ischemic optic neuropathy, central retinal artery or vein occlusion, and cortical blindness. In fact, any interruption of blood supply to the eyes during surgery--whether caused by pressure to the eye itself or to the blood supply--or an interruption to the patient's blood flow autoregulation system can lead to POVL. One study showed that there was a higher increase of intraocular pressure (IOP) in patients whose heads were supported by pillows versus patients whose heads were supported by pins in the prone position. Another study demonstrated that as time spent in the prone position increased, IOP continued to increase as well. Some authors have suggested that IOP may increase as a result of large amounts of intravenous (IV) fluids given during surgery.
A variety of factors have been identified that contribute to the various causes of POVL, some intrinsic to the patient that can be thought of as predisposing factors, while others are related more directly to surgery and anesthesia. One study concluded that consideration should be given to establishing a minimum systolic blood pressure for each patient as well as staging long procedures and protecting eye position during surgery. Other recommendations include careful preoperative history to identify any preexisting patient risk factors that predispose to POVL; considered use of deliberate hypotension in patients at risk; avoidance of compression of the eyes, abdomen, or chest in patients placed prone; and correction of anemia and/or hypotension as early as is feasible upon identification of these risk factors. The study was published in the October 2008 issue of Neuro-Ophthalmology.
"Determining the actual overall incidence of POVL is difficult since it is not known what percentage of cases is reported,” said lead author, Molly Gilbert, M.D., an assistant professor of ophthalmology at the University of Illinois Eye and Ear Infirmary. "A wide variety of surgical interventions have been associated with POVL, including cardiopulmonary bypass, lumbar spine surgery, neck dissection, abdominal procedures, hip surgery, cholecystectomy, parathyroidectomy, prostate surgery, pleurodesis, and rotator cuff surgery.”
Related Links:
University of Illinois
Latest Surgical Techniques News
- Innovation in Thermographic Neurosurgical Imaging Supports Informed Decision-Making
- Fluorescent Soft Robots Accurately Locate Early Gastric Cancer During Laparoscopic Surgery
- Ultrasound-Activated Microstructures Clean Implanted Stents and Catheters
- First-Ever MRI-Steerable Micro-Robotics to Revolutionize Glioblastoma Treatment
- Bioprinted Aortas Offer New Hope for Vascular Repair
- Early TAVR Intervention Reduces Cardiovascular Events in Asymptomatic Aortic Stenosis Patients
- New Procedure Found Safe and Effective for Patients Undergoing Transcatheter Mitral Valve Replacement
- No-Touch Vein Harvesting Reduces Graft Failure Risk for Heart Bypass Patients
- DNA Origami Improves Imaging of Dense Pancreatic Tissue for Cancer Detection and Treatment
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
Channels
Critical Care
view channel
Light-Activated Immunotherapy Combined with Engineered Protein Technology Targets Hard-To-Treat Cancer
In 2024, it was estimated that 26,890 individuals in the U.S. would be diagnosed with stomach cancer, and 10,880 would succumb to the disease. For many, stomach cancer is diagnosed too late, by which time... Read more
AI-Enabled ECG Algorithm Enables Early Detection of Heart Failure
Heart failure is a common condition in Sub-Saharan Africa, where it affects younger individuals and is often associated with poorer outcomes compared to high-income countries. Early detection of left ventricular... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more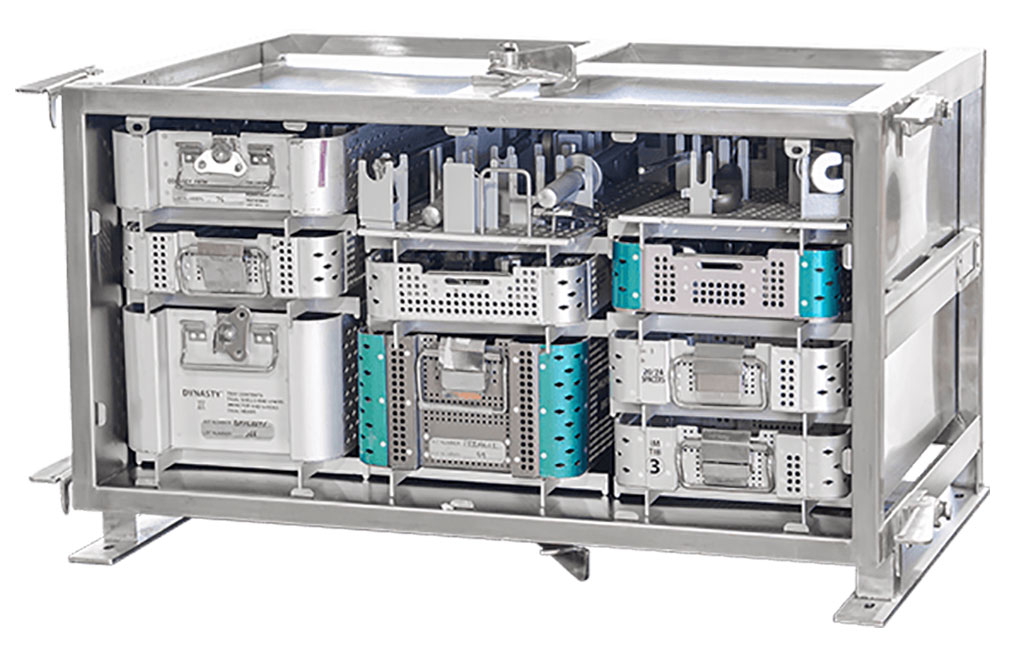
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more