No Added Benefits for Full-Defrag Ablation for AF
|
By HospiMedica International staff writers Posted on 30 Dec 2015 |
A stepwise approach to ablation for persistent atrial fibrillation (AF) does not offer any benefits over pulmonary vein isolation (PVI) alone, according to a new study.
Researchers at University Medical Center Hamburg-Eppendorf (UKE; Germany), University Hospital Cologne (Germany), and other institutions conducted a study involving 205 patients (151 men; mean age 61.7 years) who underwent de novo ablation for persistent AF. Subsequently, the patients were prospectively randomized to either PVI alone (78 patients), or full defragmentation ablation (75 patients), consisting of PVI, ablation of complex fractionated electrograms, and additional linear ablation lines. The remaining 52 patients were not randomized due to AF termination with the original PVI.
The primary endpoint of the study was recurrence of any atrial tachycardia (AT) after a blanking period of three months. The results showed that during the entire study, 241 ablations were performed. At 12 months, the incidence of AT was similar between recipients of PVI alone and those who underwent full defragmentation (8.2% versus 8.5%, respectively). Arrhythmia-free survival rates were also similar between groups, at 63.9% with PVI only and 57.7% with full defragmentation.
The researchers also found, conversely, that despite the fact that the rate of major complications did not differ materially between groups, the full defragmentation arm suffered a 23.3% incidence of pericardial effusion with symptoms of pericarditis, compared with a much lower 5.3% incidence in their single-procedure counterparts. The study was published on December 22, 2015, in the Journal of the American College of Cardiology.
“Pulmonary vein isolation should be the initial strategy in patients with persistent AF undergoing catheter ablation, because more extensive ablation is associated with longer procedure duration, fluoroscopy, and radiofrequency exposure, without better rhythm control outcomes,” concluded lead author Julia Vogler, MD, of University Heart Center Hamburg, and colleagues. She added, however, that “pulmonary vein isolation alone appears to be insufficient for treating persistent AF, with disappointing long-term results.”
PVI is a catheter ablation technique developed to prevent focal triggers in the pulmonary veins from initiating episodes of AF. Although the procedure initially involved focal ablation with a catheter directly in the pulmonary veins, isolating the pulmonary veins by applying ablation energy at their junction with the left atrium is more effective. The PVI procedure is most suitable for patients whose recurring symptomatic episodes of AF have not been suppressed by anti-arrhythmic drugs, or who do not wish to take long-term anti-arrhythmic or anticoagulation medications.
Related Links:
University Medical Center Hamburg-Eppendorf
University Hospital Cologne
Researchers at University Medical Center Hamburg-Eppendorf (UKE; Germany), University Hospital Cologne (Germany), and other institutions conducted a study involving 205 patients (151 men; mean age 61.7 years) who underwent de novo ablation for persistent AF. Subsequently, the patients were prospectively randomized to either PVI alone (78 patients), or full defragmentation ablation (75 patients), consisting of PVI, ablation of complex fractionated electrograms, and additional linear ablation lines. The remaining 52 patients were not randomized due to AF termination with the original PVI.
The primary endpoint of the study was recurrence of any atrial tachycardia (AT) after a blanking period of three months. The results showed that during the entire study, 241 ablations were performed. At 12 months, the incidence of AT was similar between recipients of PVI alone and those who underwent full defragmentation (8.2% versus 8.5%, respectively). Arrhythmia-free survival rates were also similar between groups, at 63.9% with PVI only and 57.7% with full defragmentation.
The researchers also found, conversely, that despite the fact that the rate of major complications did not differ materially between groups, the full defragmentation arm suffered a 23.3% incidence of pericardial effusion with symptoms of pericarditis, compared with a much lower 5.3% incidence in their single-procedure counterparts. The study was published on December 22, 2015, in the Journal of the American College of Cardiology.
“Pulmonary vein isolation should be the initial strategy in patients with persistent AF undergoing catheter ablation, because more extensive ablation is associated with longer procedure duration, fluoroscopy, and radiofrequency exposure, without better rhythm control outcomes,” concluded lead author Julia Vogler, MD, of University Heart Center Hamburg, and colleagues. She added, however, that “pulmonary vein isolation alone appears to be insufficient for treating persistent AF, with disappointing long-term results.”
PVI is a catheter ablation technique developed to prevent focal triggers in the pulmonary veins from initiating episodes of AF. Although the procedure initially involved focal ablation with a catheter directly in the pulmonary veins, isolating the pulmonary veins by applying ablation energy at their junction with the left atrium is more effective. The PVI procedure is most suitable for patients whose recurring symptomatic episodes of AF have not been suppressed by anti-arrhythmic drugs, or who do not wish to take long-term anti-arrhythmic or anticoagulation medications.
Related Links:
University Medical Center Hamburg-Eppendorf
University Hospital Cologne
Latest Surgical Techniques News
- Pioneering Sutureless Coronary Bypass Technology to Eliminate Open-Chest Procedures
- Intravascular Imaging for Guiding Stent Implantation Ensures Safer Stenting Procedures
- World's First AI Surgical Guidance Platform Allows Surgeons to Measure Success in Real-Time
- AI-Generated Synthetic Scarred Hearts Aid Atrial Fibrillation Treatment
- New Class of Bioadhesives to Connect Human Tissues to Long-Term Medical Implants
- New Transcatheter Valve Found Safe and Effective for Treating Aortic Regurgitation
- Minimally Invasive Valve Repair Reduces Hospitalizations in Severe Tricuspid Regurgitation Patients
- Tiny Robotic Tools Powered by Magnetic Fields to Enable Minimally Invasive Brain Surgery
- Magnetic Tweezers Make Robotic Surgery Safer and More Precise
- AI-Powered Surgical Planning Tool Improves Pre-Op Planning
- Novel Sensing System Restores Missing Sense of Touch in Minimally Invasive Surgery
- Headset-Based AR Navigation System Improves EVD Placement
- Higher Electrode Density Improves Epilepsy Surgery by Pinpointing Where Seizures Begin
- Open-Source Tool Optimizes Placement of Visual Brain Implants
- Easy-To-Apply Gel Could Prevent Formation of Post-Surgical Abdominal Adhesions
- Groundbreaking Leadless Pacemaker to Prevent Invasive Surgeries for Children
Channels
Critical Care
view channel
Ingestible Smart Capsule for Chemical Sensing in the Gut Moves Closer to Market
Intestinal gases are associated with several health conditions, including colon cancer, irritable bowel syndrome, and inflammatory bowel disease, and they have the potential to serve as crucial biomarkers... Read moreNovel Cannula Delivery System Enables Targeted Delivery of Imaging Agents and Drugs
Multiphoton microscopy has become an invaluable tool in neuroscience, allowing researchers to observe brain activity in real time with high-resolution imaging. A crucial aspect of many multiphoton microscopy... Read more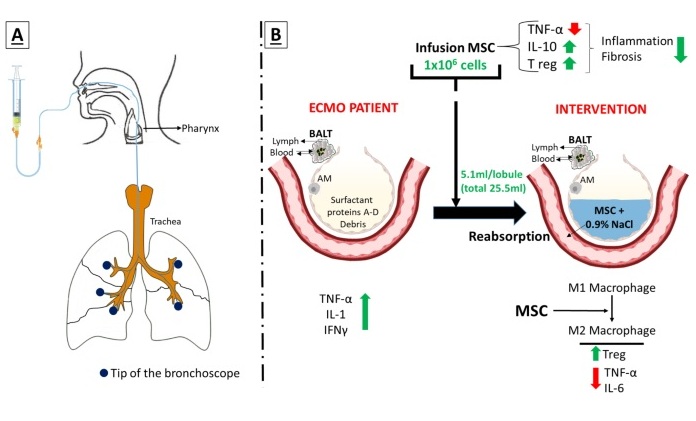
Novel Intrabronchial Method Delivers Cell Therapies in Critically Ill Patients on External Lung Support
Until now, administering cell therapies to patients on extracorporeal membrane oxygenation (ECMO)—a life-support system typically used for severe lung failure—has been nearly impossible.... Read morePatient Care
view channel
Portable Biosensor Platform to Reduce Hospital-Acquired Infections
Approximately 4 million patients in the European Union acquire healthcare-associated infections (HAIs) or nosocomial infections each year, with around 37,000 deaths directly resulting from these infections,... Read moreFirst-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
Reducing healthcare-acquired infections (HAIs) remains a pressing issue within global healthcare systems. In the United States alone, 1.7 million patients contract HAIs annually, leading to approximately... Read more
Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization
An innovative solution has the capability to transform surgical capacity utilization by targeting the root cause of surgical block time inefficiencies. Fujitsu Limited’s (Tokyo, Japan) Surgical Capacity... Read more
Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
A groundbreaking innovation enables hospitals to significantly improve instrument processing time and throughput in operating rooms (ORs) and sterile processing departments. Turbett Surgical, Inc.... Read moreHealth IT
view channel
Printable Molecule-Selective Nanoparticles Enable Mass Production of Wearable Biosensors
The future of medicine is likely to focus on the personalization of healthcare—understanding exactly what an individual requires and delivering the appropriate combination of nutrients, metabolites, and... Read more
Smartwatches Could Detect Congestive Heart Failure
Diagnosing congestive heart failure (CHF) typically requires expensive and time-consuming imaging techniques like echocardiography, also known as cardiac ultrasound. Previously, detecting CHF by analyzing... Read moreBusiness
view channel
Expanded Collaboration to Transform OR Technology Through AI and Automation
The expansion of an existing collaboration between three leading companies aims to develop artificial intelligence (AI)-driven solutions for smart operating rooms with sophisticated monitoring and automation.... Read more